This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Glaucoma affects more than 70 million people worldwide. Glaucoma is a progressive optic neuropathy characterized by alteration of the optic nerve endings and damage to the visual field, resulting from loss of retinal ganglion cells by cell apoptosis. The following article shows how Helicobacter is related to glaucoma?
1. The role of mitochondria in eye cells
Accumulated mitochondrial genome (mtgenome) damage is associated with increased cellular stress and organelle dysfunction. The filamentous reticular cells of patients with primary open-angle glaucoma (POAG) have lower ATP levels, as their function is threatened by an intrinsic mitochondrial complex defect that renders these cells deficient. mitochondrial respiration. Mitochondrial DNA (mtDNA) deletions are significantly increased in the small angular drainage canal (also called meshwork trabecular) of patients with primary open-angle glaucoma, compared with control group, and the ratio between mtDNA and nuclear DNA decreased; In addition, the amount of nuclear DNA per mg of wet tissue decreased, confirming that mitochondrial damage is severe in the small anterior angle drainage canal of patients with primary open-angle glaucoma.
The wire bundle network alters both cell motility and architecture, causes cells to die by apoptosis, loses barrier functions, and changes outflow of aqueous humor
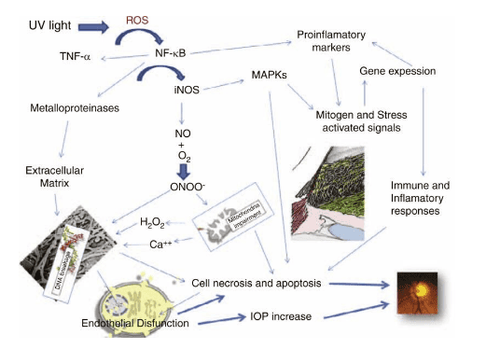
This is why Glaucoma (IOP) occurs during glaucoma. Under normal physiological conditions, about 1%–5% of oxygen consumed by mitochondria is converted to free radicals, which include superoxide anions, hydrogen peroxide, and hydroxyl radicals. Mitochondrial respiratory function declines with age, increasing the production of free radicals and free radicals in the mitochondria. Furthermore, free radicals and oxidants can act as intracellular signaling molecules, regulating cell death or survival. Broad-spectrum alterations in senescent individuals and cells are correlated with cellular responses to large doses of oxidative stress. These changes and responses include: (1) impaired mitochondrial respiratory function; (2) increase the rate of free radical production; (3) accumulation of mutations in mitochondrial DNA (mtDNA); (4) increased levels of oxidative damage to DNA, proteins and lipids; and (5) reduced degradability in oxidatively damaged proteins and other macromolecules. Responses to oxidative stress and their subsequent interactions in tissues lead to deleterious effects on cellular functions, culminating in aging and degenerative diseases. Oxidative changes and mutations in mtDNA occur very readily, and the extent of such changes in mitochondrial DNA increases exponentially with age.

Late onset and progression of age-related diseases is based on the accumulation of somatic mutations in the mtDNA of postnatal tissues
Signs of cellular senescence are found in the exit canal small water in the corner of primary open-angle glaucoma patients to a much greater extent than in age-matched controls, besides, mitochondria provide a genomic–environmental interaction between environment and genes our. The late onset and progression of age-related diseases is based on the accumulation of somatic mutations in the mtDNA of postnatal tissues. Differences in individual and regional predispositions to degenerative diseases and cancers may result from interactions between modern dietary calories and ancient mitochondrial genetic polymorphisms. . As mentioned above, free radicals are most likely the cause of small angle drainage channel disturbances, leading to glaucoma. Indeed, during primary open-angle glaucoma, the most severe small-angle drainage changes occur in the layers closest to the aqueous humor of the anterior chamber, to which the cells are in contact. with relatively high concentrations of hydrogen peroxide. Widespread and prolonged in vivo oxidative stress results in decreased corner-drain cell adhesion, loss of cells, and compromised corner-drain canal integrity.
Exceptional sensitivity of the small angle drainage channel to oxidative stress is consistent with damage induced selectively, inducing glaucoma cascade
Oxidative damage detected in the drainage canal Small water in the corner cannot explain why patients with glaucoma have low circulating glutathione levels, which suggests a general impairment of antioxidant capacity. Furthermore, the statistically significant correlation between oxidative damage to the small angle drainage channel and the increase in IOP observed in primary open-angle glaucoma cannot be explained by assuming a relationship This system is the result of drug use. Furthermore, the increase in nitric oxide synthase expression and activity in the small anterior drainage canal in primary open-angle glaucoma patients is proportional to visual field defects and may lead to increased nitrotyrosine levels, may therefore act as a marker of oxidative stress during corner drainage channel cell death. Antioxidant proteins are down-regulated with increased nitric oxide synthase 2 and in the presence of other proteins that, under physiological conditions, are cleaved inside the cell into functional mitochondria. In the pathological condition of primary open-angle glaucoma, mitochondrial proteins can be detected in AH, thus demonstrating the presence of cellular and mitochondrial damage and destruction.
Degeneration that occurs in the ocular tissues during primary open-angle glaucoma is caused by a variety of mechanisms
Degeneration occurs in the ocular tissues during primary open-angle glaucoma It is caused by a variety of mechanisms, mainly including mitochondrial damage but also inflammation, vascular dysregulation, and hypoxia. Altogether, several proteome alterations confirm the occurrence of oxidative stress in the anterior compartments of patients with primary open-angle glaucoma. In particular, the antioxidant enzymes superoxide dismutases 1/2 and glutathione S-transfer 1 in primary open-angle glaucoma patients were significantly lower in primary open-angle glaucoma patients compared with controls, while the pro-oxidative enzymes, nitric oxide synthesis 2 and glutamate ammonia ligase, were significantly higher in patients with primary open-angle glaucoma than in controls.
2. Helicobacter pylori infection is associated with glaucoma
The positive association between Hp infection and free radical production was first demonstrated in 1994. Recently, Hp bacteria were identified in trabeculum and iris samples from patients who had undergone surgery. pterygium to find primary open-angle glaucoma. Furthermore, local Hp infection induces chronic inflammation including recruitment of neutrophils and lymphocytes at the site of infection.
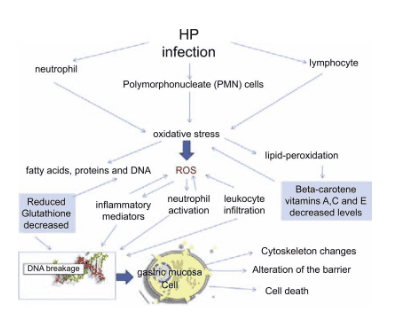
Oxidative stress is aggravated by a relative deficiency of glutathione and vitamins A, C, and E. In addition, neutrophil recruitment and release of multiple chemoreceptors/mediators cause Inflammation stimulates intense leukocyte infiltration into the gastric mucosa, which can cause tissue damage in the absence of antioxidants. This Gram-negative bacterium activates multiple oncogenic pathways in epithelial cells, including NF-kappaB, and induces epigenetic changes, such as DNA methylation and histone modification, that play an important role important in carcinogenic transformation.
Hp can be classified into two different classes based on its ability to produce cytotoxins, such as CagA (cytoxin-binding gene A) and VacA (vacuum-binding gene A)
Inside the cell , VacA can target mitochondria, at least in some cases, leading to cytochrome c release and apoptosis. Even if the actual sequence of events is not known, one potential mechanism is Hp infection to mitochondria from the endothelial cavity following accumulation, allowing a specific and direct interaction between the endothelial membrane and the endothelial membrane. and the outer mitochondrial membrane.
Mechanism of H.pylori causing glaucoma
The chain of events leading to the degeneration of endothelial cells (in glaucoma) and gastric mucosal cells (in H. pylori infection) is stress oxidation with the participation of mitochondria; This is similar in both diseases. Another similarity between the two diseases is due to an alteration in barrier function mediated by the signaling of the Rho family of GTPases. The rho-kinase pathway appears to mediate the angular small drainage channel cell responses to cyclic mechanical stress. During glaucoma, small angle drainage endothelial cell changes arise, leading to increased pressure on other molecular events, which then translate into clinical degeneration of the cells. ganglia and, consequently, damage to the visual field. Hp changes based on epithelial cell signaling and polarity, which may explain the pathogenesis of carcinoma. Finally, it is important to note the potential contribution of Helicobacter pylori infection to vascular injury. Indeed, some pathogens, such as Hp, can increase tissue factor synthesis, cell surface thrombin expression, platelet adhesion, and expression of adhesion molecules, cytokines, and cytokines. growth factors, even when reducing prostacyclin release and endothelial cell damage. Endothelial dysfunction may be one of the underlying mechanisms by which many intracellular pathogens actually contribute to these early processes leading to the development of atherosclerosis and progression to polyvascular disease. .
Hp eradication may ameliorate endothelial dysfunction
Helicobacter pylori infection stimulates the production of proinflammatory cytokines involved in the development of atherosclerosis, inducing cellular oxidative stress and dysregulation endothelial function; Furthermore, eradication of Hp can improve endothelial dysfunction. High tension glaucoma depends on endothelial cell dysfunction in the small drainage canal in the anterior chamber angle of the eye which is a real vessel that behaves as if it were a vessel, expressing all the active proteins. as an early sign of plaque atherosclerosis. However, we still do not really know whether the incidence of glaucoma in Hp-infected patients is significantly different from that in uninfected individuals.
Helicobacter pylori infection is associated with an increased risk of normotensive glaucoma (NTG)
No epidemiological studies have demonstrated a possible racial similarity and/or diversity regarding the association between Hp and glaucoma among different countries. Thus, Hp infection is associated with an increased risk of normotensive glaucoma (NTG). Indeed, retinal ganglion cells may be injured in the eye within the normal intraocular pressure range because the site of injury associated with Hp infection may be not only the fishnet meshwork but also the retinal ganglion cells. desert. It may be due to decreased ocular blood flow, secretion of toxic materials, and inflammation-induced antibody-induced apoptosis in the retrobulbar region, although the exact pathophysiology remains unclear.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.