This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalMore and more people are suffering from neuroendocrine tumor (NET) these days, especially in the gastrointestinal tract. The disease is very difficult to diagnose, mostly when it is detected at a late stage, the prognosis is severe, and treatment is difficult.
1. What is neuroendocrine tumor?
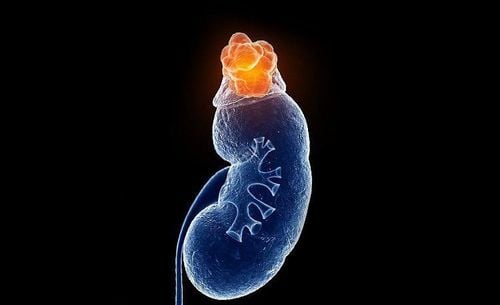
Neuroendocrine tumors are a group of diverse tumors that arise from different neuroendocrine cells in the body. Therefore, neuroendocrine tumors can arise from any part, and can be classified based on the location of appearance. In which, gastrointestinal neuroendocrine tumors are the most common primary sites of neuroendocrine tumors, including: Rectum 17.6%; small intestine 17.3%; colon 10.1%; jejunum 8%; pancreas 7.0%; stomach 6.0%.
2. What is gastric neuroendocrine tumor?
Gastrointestinal neuroendocrine tumors were formerly known as carcinoid tumors. Most gastrointestinal neuroendocrine tumors progress slowly. Most of these tumors start in the small intestine and release serotonin. Too much serotonin causes carcinoid syndrome. Gastrointestinal neuroendocrine tumors exist under two groups: highly differentiated gastrointestinal neuroendocrine tumors and poorly differentiated gastrointestinal neuroendocrine tumors.
Most gastric neuroendocrine tumors consist of ECL-like cells, typically in the body and fundus of the stomach (90%), stained with chromogranin A or synaptophysin by immunohistochemistry. There are four types of gastric carcinoids, each arising in different clinical settings, and each with a distinct prognosis and treatment regimen.
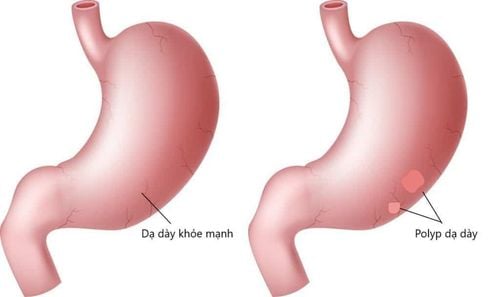
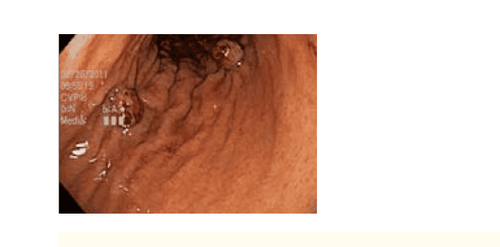
This particular tumor emphasizes the importance of parallel biopsies of the opacified mucosa. On endoscopic images, they appear as submucosal mass lesions, sometimes with ulcers.
In type I and II carcinoids, some polyps are seen in clusters, arising almost exclusively in the body mucosa. Type III lesions are usually solitary and may present throughout the stomach. Class IV carcinoids can arise anywhere in the stomach and have a significantly worse prognosis. Histologically, these neuroendocrine tumors appear similar, and biopsy of the non-polypoid mucosa is important in differentiating tumor type, prognosis, and treatment.
2.1 Type I neuroendocrine tumors
Type I neuroendocrine tumors are the most common. These occur in middle-aged women (70%-80%) and are the result of ECL cell hyperplasia arising in autoimmune atrophic gastritis (also known as autoimmune gastritis). The pathogenesis of type I neuroendocrine tumors is as follows: Autoimmune destruction of parietal cells leads to decreased gastric acid production and loss of feedback inhibition of gastrin secretion in G antagonist cells. High levels of gastrin stimulate the proliferation of ECL cells, which appear as many small nodules in the stomach body. Technically, this represents a reversible hyperplasia that can progress to malignancy, especially as the tumor enlarges.
Compared with type II and type III neuroendocrine tumors, type I lesions have a good prognosis with extremely low rates of metastatic disease. Endoscopic mucosal resection (by EMR or ESD) of any visible lesion and close endoscopic monitoring is prudent, but there are no guidelines or recommendations currently available at This is the moment and endoscopic mucosal resection is an area of future research.
Antrumectomy to remove excitatory G cells has also been shown to be useful when long-term treatment and treatment of any underlying pernicious anemia is recommended. Biopsy of the surrounding polyps is important in separating this low-risk tumor from the rest of the group.
2.2 Neuroendocrine tumors type II
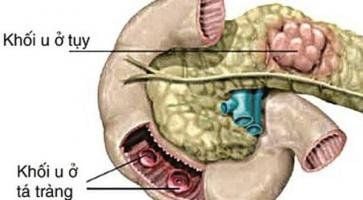
Neuroendocrine tumors of type II are rare and arise in the setting of polyendocrine malformations 1, Zollinger-Ellison syndrome, or gastrin-secreting tumors elsewhere. in the digestive tract. Uninhibited gastrin secretion stimulates ECL cells to proliferate, leading to gastric neuroendocrine tumors (usually multiple).
These type II tumors have a worse prognosis than type I tumors, with a metastasis rate in about 30% of cases. However, type II tumors performed significantly better than type III tumors, again emphasizing the importance of differentiating neuroendocrine tumor types, which can be achieved by providing biopsy specimens. and of the mucosa surrounding the lesion for the pathologist. Local excision of neuroendocrine tumors, assessment for metastatic disease, and resection of gastrin-secreting tumors (usually found in the small intestine) are the primary therapies.
2.3 Neuroendocrine tumors type III
Neuroendocrine tumors type III, 2nd most common, without associated syndrome or clinical setting; rather, these lesions are scattered, sporadic. Whereas type I and type II tumors mainly arise in the gastric body and are multiple lesions at the same time, type III tumors can arise anywhere in the stomach and are usually solitary. . In contrast to the good prognosis of type I and type II tumors, lymph node metastasis was found in 71% of type III tumors over 2 cm in size. In most cases of type III tumors, surgical resection is recommended.
2.4 Type IV neuroendocrine tumors
Type IV neuroendocrine tumors, also known as poorly differentiated neuroendocrine carcinomas, are rare solitary tumors. They can arise in any part of the stomach and occur mainly in elderly men (>60 years of age). When diagnosed, these tumors are usually large (50-70 mm), ulcerated, and are thought to result from a primary defect in acid secretion by parietal cells. Unfortunately, at the time of diagnosis, most of these tumors are already in the late stages, have extensive metastases, and have a poor prognosis.
Currently, early cancer screening is considered the perfect measure in the timely detection and treatment of all types of cancer. Reduce the cost of treatment and especially reduce the mortality rate in patients. Vinmec International General Hospital always deploys and introduces to customers Early cancer screening at Vinmec - Peace of mind to live well to help with gene testing, imaging, and biomarkers for tumor detection. Soon.
Advantages:
Only one gene test can assess the risk of 16 common cancers in both men and women (lung cancer, colorectal cancer, breast cancer, pancreatic cancer) , cervical cancer , stomach cancer , prostate cancer ,....) Early detection of early signs of cancer through imaging, endoscopy and ultrasound. The operation is simple, careful and accurate. A team of well-trained specialists, especially in oncology, are capable of handling cancer cases. With facilities, advanced and modern medical equipment and a team of doctors with deep expertise and experience. At Vinmec, the examination process becomes quick with accurate results, saving costs and time for patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.