This is an automatically translated article.
Fungal infection of the feet is a common disease in all subjects and ages. Fungal foot infections cause itching, even redness, festering and sores. Therefore, when seeing foot fungus, patients should not be subjective but need to go to medical centers soon for examination and treatment.
1. What is foot fungus?
Tinea capitis is a common fungal infection of all subjects and ages, however, the disease is more common in men, people who regularly practice sports like athletes and more often in adults than children. em.
Tinea pedis can be spread by sharing personal items or by direct contact with someone who has the fungus. The disease can appear in the form of: interstitial inflammation, keratosis, ulcers, vesicles, fungus in the toes.
2. Causes and favorable factors that cause tinea versicolor
Tinea pedis is mainly caused by Trichophyton rubrum fungus, a few other cases are caused by Candida fungus in the toes. In addition to fungi, the following factors create favorable conditions for fungi to grow, spread and infect such as:
Wet climate environments Sharing personal items such as towels Exposure in public places such as lakes swimming Frequent sweating in the feet due to high temperature, wearing tight shoes, not perspiring Have a weakened immune system or have diabetes MORE: Toenail fungus, what to do?

Mang giày dép chật là một trong các yếu tố thuận lợi gây nấm da chân
3. Manifestations of foot fungus infection
Fungal infections of the feet often appear between the toes, soles or insteps, on one or both feet, with manifestations depending on the location of the fungal infection such as:
Inflammation, itching, cracking, discharge, closure scales between the toes. Pink, red skin on the soles of the feet. Itchy, red skin, scaly keratosis, round shape, with blisters on the instep. Painful and itchy blisters, blistering skin on the soles or insteps. Fungal infections of the feet, if not treated, can cause sores due to pus-filled pustules, after drying, the crusts, thickened, cracked, painful scabs. These lesions usually appear between the toes or the soles of the feet. This serious condition is often associated with a bacterial infection. In particular, for people with weakened immune systems or diabetes, fungal foot infections often cause foot sores.
MORE: Severe atopic dermatitis on the instep, sores, discharge and itching what to do?
4. Treatment and care for foot fungus infection
4.1 Treatment of foot fungus When seeing the above symptoms and suspecting a fungal infection of the feet, the patient should visit a medical facility with a dermatology specialty to be diagnosed with the disease, from which a direction can be taken. suitable treatment. Avoid arbitrarily buying drugs to apply or take because the disease needs to be differentiated from atopic dermatitis due to contact, psoriasis or leech nests.
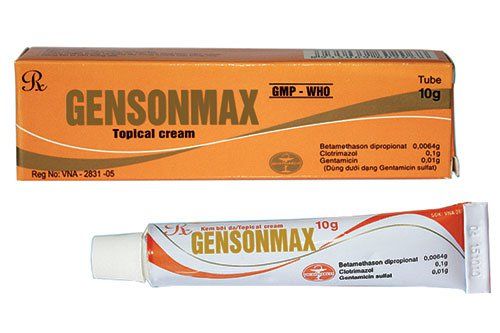
If the foot fungus infection is mild, the doctor may prescribe some antifungal cream such as Clotrimazole, Miconazole or Terbinafine for about 2 weeks.
If after 2 weeks of treatment, there is no improvement, the damaged skin does not return to normal or the pain and itching is more severe, the patient should return to the doctor to be diagnosed and prescribed other drugs, especially when pustules, blisters, ulcers appear.
The doctor may prescribe some drugs to treat foot fungus with stronger antifungal effects such as Ciclopirox, Econazole, Ketoconazole, Naftifine, Oxiconazole, Sulconazole, ... In addition, some creams and topical solutions Other options may be considered for symptomatic treatment of the disease such as:
Reduction of keratosis: A solution consisting of urea and salicylic acid or lactic acid. After applying this compound to reduce horny scales, it will create favorable conditions for the anti-fungal cream to penetrate the skin more easily and effectively. Reduces perspiration: The solution contains aluminum chloride, which reduces perspiration in the feet, helping to prevent and limit fungal infections of the feet. Reduce infection: To prevent or reduce bacterial infection, you can apply antibiotic cream. To relieve itching: To relieve itching caused by bacteria and fungi, you can apply an antihistamine. In case the use of topical drugs does not relieve the symptoms of foot fungus, it is possible to switch to oral antifungal drugs such as Fluconazole, Griseofulvin, Itraconazole, Ketoconazole, Terbinafine, ... for 3-4 weeks.

Người bệnh nấm da chân nên đến gặp bác sĩ để được điều trị kịp thời
4.2 Skin care when infected with foot fungus It is very important to take care of the skin of the feet in the following ways, to help prevent re-infection:
Always keep your feet dry and clean., Avoid creating a humid environment for fungal bacteria to form and grow. Wash your feet clean every day, after washing can use a towel to dry. Always use separate personal items, especially towels, separate towels at the feet. Use socks made of cotton fabric to help keep the skin of the feet open when wearing closed shoes. However, care should be taken to change socks to avoid creating an environment for foot fungus. Regularly use slippers, especially in public. Avoid wearing shoes made from rubber or plastic. Use powdered antifungal medication to get inside your shoes when you wear them. When you see symptoms of itching, blisters, discharge, keratosis scabs or even sores on the feet, the patient should visit a medical facility for a diagnosis and appointment of appropriate medication. physical.
With many years of experience in the examination and treatment of diseases, now Vinmec International General Hospital has become one of the major health care centers, capable of examining, screening and treating diseases. treat many serious diseases. Therefore, when there are signs of tinea pedis, patients should not be subjective but can go to Vinmec International General Hospital to examine and receive support and advice from doctors.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.