This is an automatically translated article.
Fluid resuscitation in emergency resuscitation is a very commonly used method today. It plays an important role in handling unexpected situations.
1. General overview of fluid resuscitation in emergency resuscitation
The most important thing in the treatment of traumatic shock is determining the cause and treating it accordingly. For the cases of hemorrhagic shock and hypovolemic shock in trauma, the most effective method is perfusion and fluid replacement.
Fluid response means that the patient will increase oxygen delivery to the tissues after rehydration. Fluid resuscitation should be done promptly and without delay, but it is not a substitute for complete control of bleeding. Fluid response when stroke volume (SV) or cardiac output (CO) increases >= 10%-15% after a 500 mL bolus (10 mL/kg in children)
2. Diagnosis of shock and monitoring of fluid resuscitation
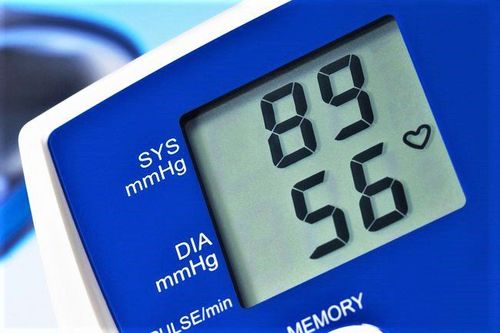
2.1 Diagnosis Shock is an inadequate tissue perfusion due to an imbalance between tissue oxygen supply and demand. Depending on the severity of the shock, different organs are affected more or less, thereby causing many different symptoms. Significant brain and heart related symptoms are present only in severe cases. Hypotension and tachycardia are not sensitive parameters for the diagnosis of shock because these may result from profound circulatory disturbances, with 25% of patients in shock having normal blood pressure and heart rate. .
Chỉ số huyết áp giảm và tim nhịp nhanh thường không có giá trị cao trong chẩn đoán sốc
2.2 Follow-up Pulmonary artery catheter (PAC) may be useful in elderly patients with severe injury, but further studies are needed to evaluate accurately. The pH, HCO3-, hypokalemia, and lactic acid values of arterial blood are suggestive of tissue hypoperfusion and persistent abnormal values reflect a poor prognosis. Therefore, these parameters would be the best predictor of shock, rather than vital signs, but have limitations in long-term evaluation.
3. Subjects who need to use rehydration therapy
The method of resuscitation in emergency resuscitation will be used in cases of shock or tissue hypoperfusion (circulatory failure). Some symptoms of this phenomenon will be manifested as:
Change in perception. Chi cold. The TRC is prolonged. Fluffy skin. Blood pressure drops. The peripheral pulse is mild, with a clear difference between the peripheral and central pulse pressures. Decreased urine output < 1 ml/kg/hour.

Chi lạnh là triệu chứng của hiện tượng suy tuần hoàn
4. Methods for predicting fluid resuscitation
Currently, methods to predict fluid response are classified into 2 types as follows:
4.1 Static method Right Atrial Pressure (RAP). Pulmonary arterial pressure (PAOP). Right ventricular end end-diastolic volume (RVEDV). Left ventricular end-diastolic volume (LVEDV). 4.2 Dynamic method Passive leg lift (PRL). Inspiratory inferior vena cava (dIVC). Pulse Pressure Variation (PPV). Variation of stroke volume (SVV). Variation of aortic valve velocity (∆Vpeak).
5. How to choose an infusion?
5.1 Crystals The “Advanced Trauma Resuscitation” program recommends giving crystalloids first. Because of the risk of metabolic acidosis due to increased chloride compared with normal saline, Ringer lactate solution is preferred for trauma patients.

Dịch truyền Ringer lactat được lựa chọn cho người bệnh chấn thương
Mass infusion of crystalloids can cause a number of effects such as: dilution of clotting factors, ARDS and increased intra-abdominal pressure. Excessive fluid resuscitation contributes to increased mortality. Crystals should be treated like any other drug in terms of indications, side effects, adverse effects and contraindications. 5.2 Hypertonic saline The theoretical benefit of hypertonic saline is to stabilize the amount of fluid entering the intravascular and interstitial spaces without significantly increasing total body water. Smaller volume replacement is allowed because the hypertonic saline redistributes into the third compartment at a slower rate. Except in the case of routine use of hypertonic saline. Hypertonic saline is an effective means of controlling intracranial pressure in traumatic brain injury patients because of the much higher concentration of sodium chloride (23.4%).
5.3 Colloidal Colloids contain proteins that allow them to remain in the lumen and create a colloidal osmotic pressure that moves fluid from the cells into the lumen. Colloids can improve microvascular perfusion, however, they are more expensive than crystalloids and are associated with many deleterious immunological effects. In case of using high doses of artificial colloids, it can lead to blood clotting disorders.

Dịch keo được truyền vào cơ thể người bệnh giúp cải thiện tưới máu vi mạch
Dextran colloid has been associated with fatal anaphylaxis, pulmonary edema, platelet dysfunction, and kidney injury.
Several trials and meta-analyses over the past 10 years have demonstrated no difference in outcomes in resuscitated patients using crystalloid and colloidal resuscitation.
The method of rehydration for patients with hypovolemic shock and hemorrhagic shock can be an important factor affecting treatment outcome.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.