This is an automatically translated article.
The article was written by Specialist Doctor I Tran Ngoc Thuy Hang - Resuscitation - Emergency Doctor, Emergency Department - Vinmec Central Park International General Hospital.Asthma is a disease characterized by chronic inflammation of the bronchial mucosa, which increases the bronchi's frequent response to many stimuli, leading to diffuse constriction of bronchial smooth muscle. Bronchospasm is not permanent, usually reversible either spontaneously or after administration of a bronchodilator.
1. What is bronchial asthma?
Asthma clinically presents with symptoms of wheezing, dyspnea, chest tightness and cough. These symptoms will vary in frequency and intensity each time they appear. These symptoms are related to changes in exhaled airflow due to bronchoconstriction, airway wall thickening, and increased secretion of viscous sputum.
1.1 Definition of asthma exacerbation An asthma exacerbation is the worsening of symptoms of dyspnea, cough, wheezing, chest tightness, and decreased lung function. Exacerbations can occur in patients with already diagnosed asthma or, sometimes, as the first manifestation of asthma. Exacerbations often occur in response to exposure to extrinsic factors (eg, upper respiratory viral infections, pollen or pollutants) and/or poor adherence to controller medications. Exacerbations can occur while the patient is being treated for asthma. When asthma is not controlled, especially in high-risk patients, the frequency of asthma attacks is high and the severity also increases, which can lead to death.

Đợt cấp hen phế quản người bệnh xuất hiện triệu chứng ho và khó thở
1.2 Factors that trigger asthma attacks and aggravate asthma symptoms Viral infections, infections Domestic and occupational allergens: house mites, house dust, pollen, cockroaches, smoke tobacco, cosmetics, weather changes, stress, strenuous exercise. Several drugs can trigger an asthma attack: beta-blocker ; aspirin and some other NSAIDs. Exacerbations of comorbidities: heart failure, myocardial infarction, diabetes, . . . . 1.3 Diagnostic criteria: Two basic features of bronchial asthma (1) History of respiratory symptoms such as wheezing, dyspnea, chest tightness, and cough. Disease manifestations vary over time, severity, AND
(2) Variable expiratory airflow limitation, confirmed at least once.
Diagram of clinical diagnosis of bronchial asthma according to GINA (2019)
| 1. Bệnh sử: có các triệu chứng hô hấp thay đổi: |
|
Các triệu chứng điển hình là thở khò khè, khó thở, nặng ngực và ho. - Người bị hen thường có nhiều hơn một trong các triệu chứng nêu trên - Các triệu chứng biến đổi theo thời gian và cường độ - Các triệu chứng thường xảy ra hoặc nặng hơn vào ban đêm hay lúc thức giấc - Các triệu chứng thường khởi phát khi gắng sức, cười lớn, tiếp xúc các dị nguyên hay không khí lạnh - Các triệu chứng thường xảy ra hoặc trở nên xấu đi khi nhiễm vi rút |
| 2. Bằng chứng về sự biến đổi giới hạn dòng khí thở ra: thể hiện bằng hô hấp ký |
|
- Ít nhất một lần trong quá trình chẩn đoán có FEV1 thấp, ghi nhận tỉ lệ - FEV1/FVC thấp hơn giá trị bình thường thấp. Tỉ lệ FEV1/FVC bình thường lớn hơn 0,75-0,80 đối với người lớn và hơn 0,85 đối với trẻ em. - Ghi nhận biến đổi chức năng hô hấp cao hơn ở người khỏe mạnh. Ví dụ: + FEV1 tăng hơn 12% và 200mL so với giá trị ban đầu (ở trẻ em, >12% giá trị dự đoán) sau khi hít thuốc giãn phế quản. Được gọi là “giãn phế quản hồi phục”. + Trung bình hằng ngày LLĐ thay đổi >10% (ở trẻ em, >13%) + FEV1 tăng hơn 12% và 200mL so với giá trị ban đầu (ở trẻ em, >12% giá trị dự đoán) sau 4 tuần điều trị bằng thuốc kháng viêm (ngoài các đợt nhiễm trùng hô hấp) - Sự thay đổi vượt mức càng lớn trong nhiều lần đánh giá thì việc chẩn đoán HPQ càng chắc chắn hơn. - Việc thăm dò nên được lặp lại trong khi có các triệu chứng, vào sáng sớm hay sau khi sử dụng các thuốc giãn phế quản. - Hồi phục phế quản có thể không thấy trong đợt cấp nặng hay nhiễm vi rút. Nếu hồi phục phế quản không thấy trong thăm dò chức năng hô hấp lần đầu, thì bước tiếp theo phụ thuộc vào tính cấp bách của lâm sàng và sự sẵn có của các thăm dò khác. - Làm thêm các thăm dò khác để hỗ trợ chẩn đoán, bao gồm cả thử nghiệm gây co thắt phế quản. |
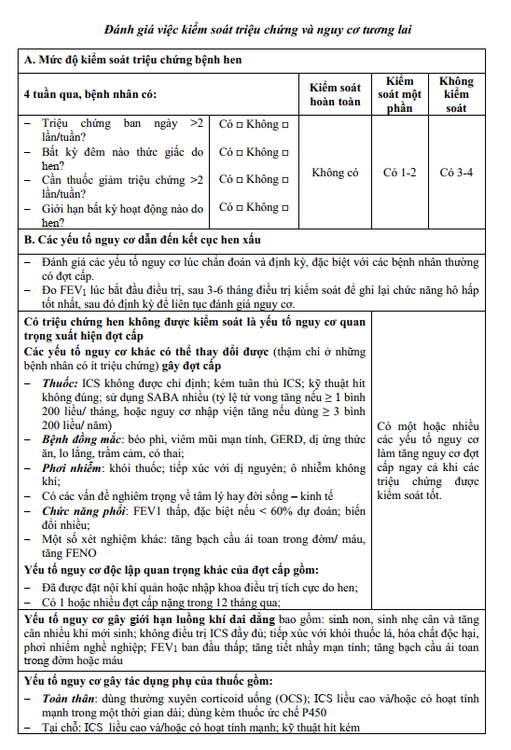
1.4 Assess asthma control
2. Treatment of bronchial asthma
Treatment of asthma exacerbations Management of asthma: treatment of symptom control, prevention of risk factors for asthma onset, loss of lung function, side effects of treatment drugs. 2.1 Long-term asthma medications are divided into 3 main categories Asthma controller drugs: are maintenance drugs used to treat asthma that reduce the risk of exacerbations and decline in respiratory function by reducing inflammation. airway. Asthma relievers: are drugs used only to relieve asthma and relieve symptoms, when the patient has a shortness of breath or an asthma attack. Reducing the need or absence of asthma relievers is an important goal of asthma treatment. Combination therapy for severe asthma: these are considered when a patient has persistent asthma symptoms and/or exacerbations despite optimized treatment with high-dose ICS (inhaled corticosteroids) / LABA (long-acting β2 agonist) and risk factors were prevented.
2.2 Emergency Treatment of an Asthma Exacerbation Assess the severity of the exacerbation: degree of dyspnea (inability to speak, or say words), respiratory rate, pulse, SpO2, and pulmonary ventilation function ( or labor force). Evaluation of other causes of acute dyspnea: heart failure, upper respiratory tract disease, aspiration of foreign bodies, pulmonary embolism... Initiation of treatment:
Oxygen inhalation: titrated dose should be used. Maintain SpO2 93-95% (94-98% for children 6-11 years old). Short-acting bronchodilators: preferred. Increase dose, and frequency of SABA administration (usually with spacer or nebulizer); Systemic corticosteroids: 1 mg prednisolone (or equivalent)/kg/day for adults, up to a maximum of 50 mg/day, and 1-2 mg/kg/day for children 6-11 years old to a maximum of 40 mg/day day. Systemic corticosteroids should be used for 5-7 days. Corticosteroids inhaled, nebulized (budesonide or fluticasone): dose 2mg-4mg/day nebulized for adults and dose 1mg-2mg/day for children. Controller: dose should be increased over 2-4 weeks. If no controller is currently in use: therapy with a stable dose of ICS should be initiated. Antibiotics: only used if the cause of the exacerbation is an infection. Assess response frequently: reduce oxygen dose and maintain SpO2 93-95%.
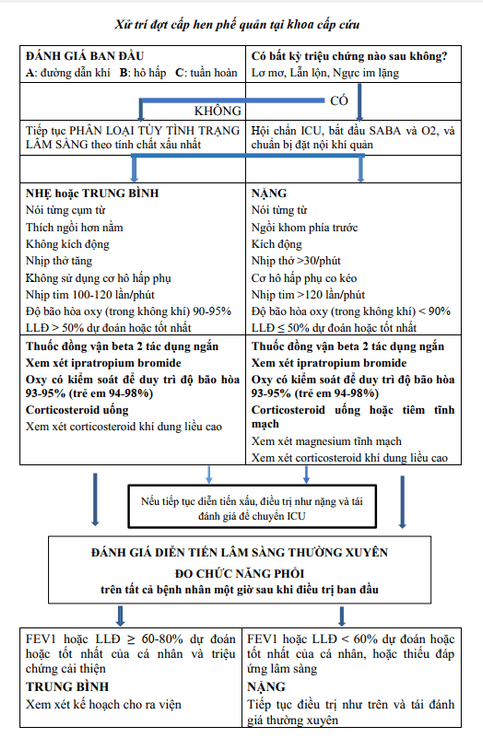
2.3 Evaluation of treatment response Routine assessment of clinical response, SpO2. Pulmonary function can be measured when the patient is relatively stable.
In case the patient has a serious development: Intensive treatment specialist.
2.4 Look for factors that contribute to symptoms and exacerbations Look for modifiable factors that contribute to symptoms or exacerbations:
Incorrect inhalation technique. Compliance is not good. Comorbidities: anxiety and depression, obesity, reduced physical activity, chronic nasopharyngitis, induced laryngeal obstruction, GERD, COPD, sleep apnea, bronchiectasis, heart disease, and kyphosis due to osteoporosis. Modifiable risk factors and triggers such as cigarette smoking, exposure to secondhand smoke, and sensitization to allergens, air pollution, molds, toxic chemicals, etc. Use of SABAs frequently frequently or excessively, causing decreased responsiveness and increased demand for use. Difficult social and economic problems: may contribute to poor adherence to treatment. Drug side effects: may contribute to reduced adherence to treatment.

Người bệnh đồng mắc béo phì có thể góp phần gây ra triệu chứng và đợt cấp
To proactively prevent disease, customers can refer to the Asthma Screening Package of Vinmec International Hospital to help:
Screen for early detection to promptly control and treat the disease Perform clinical examination , taking medical history, measuring respiratory function, otolaryngology examination and screening for bronchial asthma.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Abbreviations: ICS: inhaled corticosteroid, inhaled corticosteroid; ICU: Intensive Care Unit (ICU) ; IV: intravenous injection; O2: oxygen; LLD: peak expiratory flow; FEV1: forced expiratory volume in the first 1 second; SABA: Short-acting beta-2 Agonist (short-acting beta-agonist); LABA: Long-acting beta-2 Agonist (long-acting beta-agonist), SAMA: Short-acting muscarinic antagonists (short-acting antimuscarinic drug).
Reference documents: Decision No. 1851/QD-BYT of the Ministry of Health issued on April 24, 2020 on the professional document "Guidelines for the diagnosis and treatment of asthma in adults and children over 12 years old". "; GINA 2019.