This is an automatically translated article.
Articles written by MSc, BS. Nguyen Van Huy, Emergency Resuscitation Department, Vinmec Ha Long International General Hospital
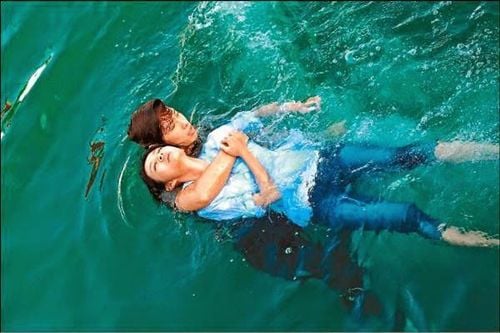
Asphyxiation can happen to anyone, even proficient swimmers can drown. If not treated promptly and properly, the mortality rate is very high. So what is the correct way to give first aid to asphyxiation?
Asphyxiation, also known as drowning, is very common, especially in the summer. Drowning can happen to anyone, from children, teenagers to adults. Especially the tourist places to swim, swim in pools, rivers and lakes. Mortality as a result of asphyxiation is often high due to inadequate or inadequate first aid treatment. In the US, about 5,000 people drown each year (80% due to lack of preventive and protective measures, 40% are children < 4 years old).
Favorable factors :
Small age; Can not swim; Drinking alcohol; Drug poisoning; Injury; Epilepsy ; Sometimes due to subjectivity, drowning in both good swimmers and rescuers. Asphyxiation with inhalation of water into the lungs: 90% of victims.
Asphyxiation without breathing water into the lungs: 10% of victims.
1. Pathophysiology
1.1 Three common drowning situations
Asphyxiation due to exhaustion or inability to swim. Asphyxiation (water splash, water shock) due to fainting on contact with water. + Due to injury:
. Pressure on epigastrium, eyeball, genital area
. Sudden flexion or extension of the cervical spine
+ Due to heat or heat difference
. Thermal shock: Increased temperature causes vasodilation, reducing effective circulating volume
. Immersion in cold water: Sudden vasoconstriction, causing a sudden increase in cardiac volume
+ Due to allergies (rare):
. Allergy to cold, to water, to algae...
. Often there are urticaria, edema of the pharynx and larynx
+ Due to fear (usually in children)
Asphyxiation during diving + Syncope due to ear pressure trauma;
+ Syncope due to increased intrathoracic pressure (not wearing a diving suit);
+ Inspiratory reflex after prolonged holding of breath;
+ Brain ischemia due to respiratory alkalosis;
+ Syncope due to parasympathetic reflex (Valsalva maneuver);
+ Accident due to pressure drop too fast;
+ Nitrogen poisoning;
+ Divers' oxygen poisoning.
1.2 Four stages of asphyxia (experimental studies)
Each stage lasts about 1 minute.
Stage 1 - Reflex apnea due to sudden closure of the pharynx: Slow heart rate and increased blood pressure. Stage 2- Return of breathing (due to increased CO) leading to aspiration of water: Coma and convulsions begin. Stage 3 - Apnea and pulse collapse. Stage 4 - Cardiac arrest: Usually occurs 3-6 minutes after being submerged in water. Lift the patient up at stage 1,2,3: the patient can breathe on his own.
If the patient is submerged in water for 7-10 minutes or more: risk of irreversible brain damage (except for very cold drowning, the low temperature will last longer: 10-30 minutes).

1.3 Consequences after asphyxiation
1.3.1 Lung damage
Sea water (hypertonic): Water from the blood vessels is pulled into the alveolar lumen, leading to: + Very early pulmonary edema.
+ Increased intrapulmonary shunt (due to hypoventilation of alveoli due to fluid filled, while blood vessels in the lungs are still guaranteed perfusion).
Fresh water (hypotonic) + Water in the alveolar lumen is absorbed into the circulation and then rapidly redistributed throughout the body. Dilute with the victim's blood.
+ Damage to surfactant causes atelectasis of the lungs and disturbs the ventilation/perfusion ratio. As a result, there is also an increase in shunts in the lungs.
+ There is also a risk of lung damage due to chemicals dissolved in water: Chlorine in swimming pool water can cause early and severe pulmonary edema.
In summary, whether fresh or salt water asphyxiation leads to:
+ Increased shunt in the lungs, pulmonary edema, congestion, brain hypoxia, hypoxia of target organs.
+ Severe brain hypoxia easily causes pulmonary edema by neurological mechanism.
1.3.2 Water and electrolytes
Increases blood volume and decreases blood sodium if large amounts of hypotonic soft drinks are inhaled. Hypovolemia and hypernatremia if large quantities of hypertonic saline are inhaled. In fact, severe fluid and electrolyte disturbances are rare in patients who are still alive at the time of admission to the emergency room. Usually, patients with transient hypervolemia at first (within 1 hour) will then experience hypovolemia due to volume redistribution in the following hours and days. Only in a small number of patients (< 15%) had marked fluid and electrolyte disturbances and hemolysis due to aspiration of large quantities of water (> 22 ml/kg). Most of these cases are very severe and do not recover after CPR. However, it should be noted that some patients drink quite a bit of water. These patients are prone to severe water and electrolyte disturbances and are at high risk of aspiration of gastric juice into the lungs during emergency.
2. Symptoms and prognostic significance
2.1 Neurological symptoms
Reflects hypoxia. Various conditions:
Hypotonic coma, loss of tendon reflexes: very poor prognosis. Hypertonic coma (cortical loss, brain loss): poor prognosis. Convulsions: risk of aggravation of cerebral edema, metabolic disorders. Mild cases: can be discharged after a few hours, but the state of excitement, confusion, headache, visual disturbance persists for several hours or days. Neurological symptoms may be aggravated secondary (after 2 days to 1 week) by the presence of cerebral edema (due to hypoxia, cerebral ischemia) and by demyelinating postanoxic demyelination.

2.2 Respiratory symptoms
The patient usually quickly resumes breathing on his own after being picked up. The prognosis is very severe if the patient does not breathe on his own.
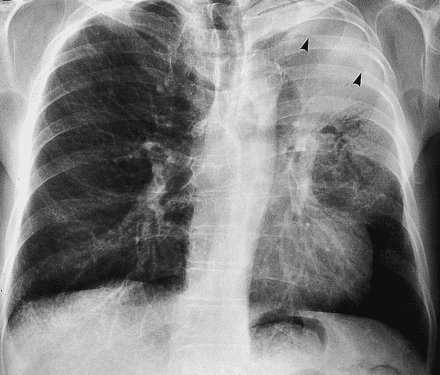
Acute pulmonary edema:
Rapid breathing, purple Sputum spitting up pink foam Ran moist in both lungs X-ray: blurred wings on both lungs Lung damage will improve after a few days, but may worsen secondary (needs monitoring) Monitor for at least 48 hours) Patients at high risk of ARDS, especially in case of inhalation of dirty water Risk of bronchial obstruction, atelectasis due to foreign bodies (moss, algae, etc.), lung infection if water is inhaled dirty. The risk of pneumonia is great. usually anaerobic bacteria from mud, soil, dirty water such as Hydrophila Aeromonas, Whitmore...etc.
2.3 Cardiovascular symptoms
Arrhythmias:
Bradycardia, tachycardia, extrasystoles (usually resolves when hypoxia is over) Ventricular fibrillation (rarely recorded), asystole. Acute heart failure:
Myocardial ischemia (due to severe hypoxia), even MI if there is pre-existing underlying coronary artery damage. There is often vasoconstriction due to hypovolemia, hypoxia, and heart failure. CVP is usually transiently elevated during the first hour, then returns to normal or low. Severe cases require monitoring and evaluation of hemodynamic parameters and intensive intensive care when entering the ICU.

2.4 Other symptoms
Possible renal failure due to acute tubular necrosis due to hypoxia, prolonged vasoconstriction, hemoglobulinuria if hemolysis is present. Patients often have hypothermia on admission and temperature disturbances, high fever in the later stages. The stomach is often full of water, there is a risk of vomiting and aspiration of gastric juice into the lungs.
2.5 Biochemical tests and blood gases
Usually hemoconcentration, rarely hemolysis Rarely changes in blood electrolytes Often has a reaction of hyperglycemia and leukocytosis Blood gases: PaO2 decreased, depending on the extent of lung damage after suffocation. can be very heavy, or stable. Acidosis: mixed acidosis at first, then metabolic acidosis when the patient resumes breathing or is on mechanical ventilation
3. Handling
3.1 On-site first aid
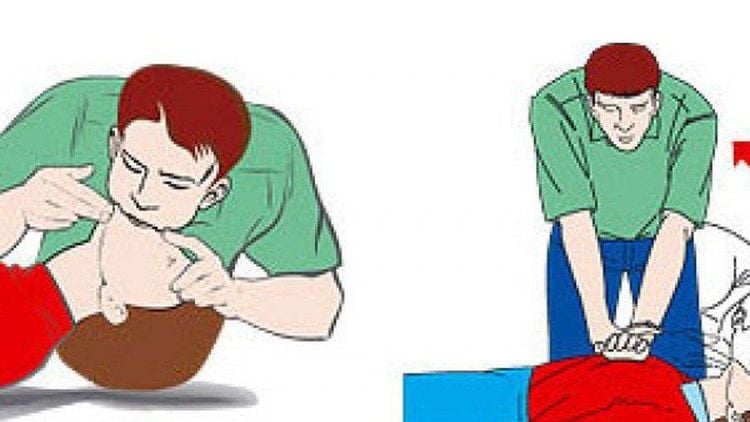
Main objective: CPR.
Quickly get the patient out of the water using appropriate field measures. Hook the throat to remove the foreign body (if any) and perform artificial respiration immediately. As soon as possible if the patient loses consciousness, coma, stops breathing, stops circulation. Perform chest compressions as soon as possible if cardiac arrest occurs. If cervical spine injury: should be fixed and cautious when moving. Sometimes cervical spine injury is the cause of drowning. Quickly transport the patient to the hospital: + Continue to maintain cardiopulmonary resuscitation (if necessary).
+ Give oxygen if the patient can breathe on their own.
Note: should not do the reverse slope of the victim because: + This method only works to clear the throat and mouth
+ Usually there is only a little water in the lungs and if it is fresh water, it will be absorbed immediately Few minute .
+ The risk of aspiration into the lungs is increased if these measures are not recommended.
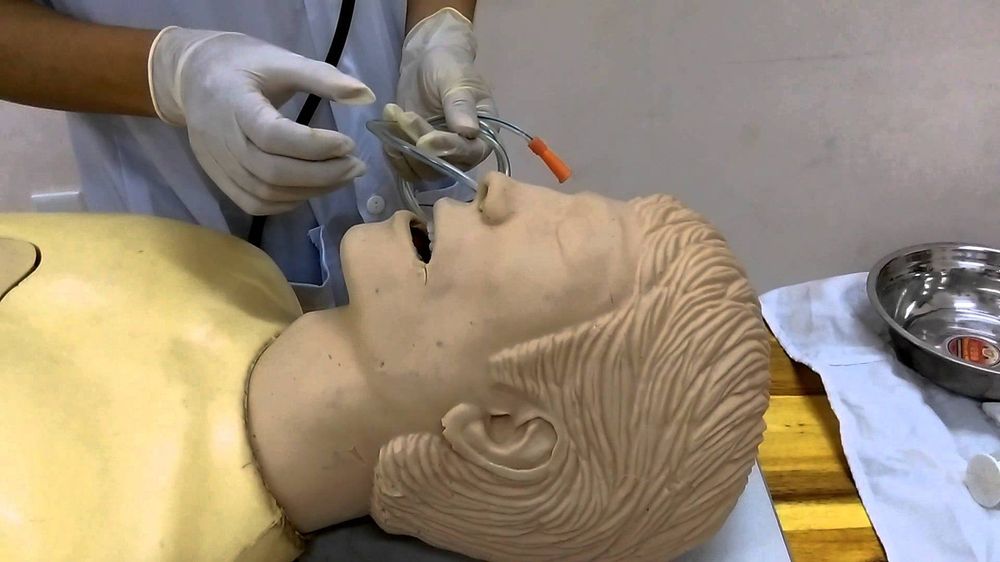
3.2 At the hospital
Reassess first aid effectiveness. Treat respiratory failure and accompanying lesions in the following hours and days.
3.2.1 Ensure ventilation and oxygen
High PEEP pulmonary protective ventilation with severe ARDS pneumonia as a result of drowning days later. Perform lung opening maneuvers to ensure targeted alveolar ventilation every 4 hours, to ensure optimal PEEP is maintained, or CPAP if the patient is breathing spontaneously (effect reduces intrapulmonary shunts and reduces pulmonary edema) . More severe requires cardiopulmonary bypass (ECMO). Targeted hypothermia protects the brain, protects nerves, stabilizes metabolic disorders if there is a deep coma as a result of asphyxiation. Target: target PaO2> 80 mmHg, PaCO2 = 30-35 mmHg. Note: PEEP must be reduced gradually when wanting to remove PEEP, because abrupt PEEP removal can cause recurrent pulmonary edema.
Mild cases: Lying in bed for 24-48 hours (preventing late pulmonary edema due to heart failure) Oxygen, monitoring SpO2 and blood gases. Appropriate treatment of heart failure. Bronchodilators if there is bronchospasm. Daily chest X-ray to evaluate the progression of severe lung injury.

3.2.2 Ensure hemodynamics
Should limit fluid to about 1-1.5 liters/24 hours. Depending on the specific NB situation. If there is vascular collapse: + Insert venous catheter, hemodynamic investigation.
+ Infusion based on intravascular pressure. Or according to the hemodynamic parameters.
+ If BP is still low: use appropriate cardiac inotropes and vasopressors.
Should not give lasix while having hypovolemia and hemoconcentration
3.2.3 Against cerebral edema and convulsions
Lie down 30o with your head high. Give hyperventilation Avoid fluid infusion and possibly use Lasix. Mannitol 20% 1 g/kg IV over 15 min/every 6 h. sedatives, reducing brain metabolism such as: Phenobarbital, Thiopental
3.2.4 Other actions and measures
Put intubation, suction gastric juice. Heat if hypothermia, bring temperature above 34oC. If high fever: paracetamol and cold compress head and neck. Record ECG, chest X-ray, blood gas test, CK, hemoglobinuria. Bicarbonate if the metabolic acidosis is severe. Pay attention to blood sugar regulation. Thrombosis prevention. Antibiotics if there is aspiration pneumonia. Pay attention to gram-negative anaerobes. Augmentin, Metronidazole, Levofluxaxin, Tazocin...etc. Can add aminosides. Usually do not take antibiotics if there is no infection. Corticosteroids: not recommended.
4. Prognosis
Bad prognosis if: Late detection, long immersion in water, late emergency, inappropriate.
Submergence time > 5 minutes; Glasgow at entry < 5 points; Dilated pupils, loss of light reflexes; Cardiac arrest, respiratory arrest on admission; Blood pH at hospital admission < 7.1. Asphyxiation has a high mortality rate, drowning prevention measures, knowledge of drowning risks for everyone is most important, and if drowning victims are detected early, Early first aid, correct and appropriate first aid, severe cases requiring good and active treatment at intensive care facilities will help to successfully cure and reduce mortality.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.