This is an automatically translated article.
Posted by Doctor Bui Thi Hong Khang - Laboratory Department - Vinmec Central Park International Hospital
While sloughing cytology is based on natural or artificial sloughing cells for diagnosis, aspiration cytology is based on cells aspirated from organ tissues with a fine needle (with a fine aperture). glass ≤ 22G).
1. History
From the mid-19th century to the early 20th century, there were scattered reports by physicians such as Kn (1847), and Ménétrier (1887) in France, Hans Hirschfield (1912) in Germany, about needlesticks. fine needle cytology to diagnose lung tumor, skin lymphoma. In 1933, the team of Hayes Martin, Edwards Eillis and Fred Steward of Memorial Cancer Hospital in New York, had a report summarizing the experience of diagnosing tumors by aspiration cytology with 2500 cases. However, aspiration cytology was still not widely available in the United States because most surgeons at that time still did not believe in the accuracy of the diagnosis, even fearing the possibility of spreading cancer cells. letter by way of suction. In contrast, in Europe especially Sweden, in the period 1950-1970; fine-needle aspiration cytology has received increasing attention from the medical world, having developed strongly with such names as Nils Suderström, Sixten Franzen and Torsten Luwhagen, of Karolinska hospital - Stockholm (Figure 1. ).
Their experience of aspiration cytology of neoplasms, especially those of the mammary gland, salivary gland and thyroid gland, has been transmitted around the world (including USA), through intermediaries of international students studying in Sweden; thereby spurring the re-emergence of fine needle aspiration cytology. In general, this is a technique with many advantages such as safety, less time and money, but high accuracy, from 90-99%. However, it must be emphasized that this technique only plays a supplementary role, but does not completely replace the routine histopathological technique, in the process of disease diagnosis for appropriate treatment.

2. Indications and contraindications
The main goals of aspiration cytology are to determine the benign/malignant nature and distinguish the origin of the neoplasm from the tumor type. Thus, fine needle aspiration cytology can be indicated for all palpable tumors; For tumors that are too small to be felt or are located deep in the body, previously unable to be aspirated, it can now be done with the help of ultrasound, endoscopic-ultrasound, computed tomography. Although there are few absolute contraindications; However, it is also not recommended to perform aspiration cytology in the following cases:
Carotid tumor and choriocarcinoma (can cause syncope and high blood pressure). Ovarian cyst (risk of spreading tumor cells in the peritoneal cavity). Parasitic cysts (can cause anaphylaxis) Tumors located deep in the area prone to bleeding (hemophilia, taking anticoagulants).
3. Executor
Fine-needle aspiration cytology can be performed by a clinician, radiologist (ultrasound, computed tomography), pathologist or cytologist; No matter who they are, they must have the skills to ask questions and do a clinical examination (to understand the history, medical history and determine the location to be aspirated), have full knowledge of anatomy (to avoid damage to vascular-neuro-vascular structures during aspiration). If the aspirator is also the person reading the cytology, this is ideal, because it will reduce the rate of false-negative results (due to incorrect puncture site, specimen not meeting diagnostic criteria, etc.). ...).
4. Performing fine needle aspiration technique
4.1 Prepare the patient:
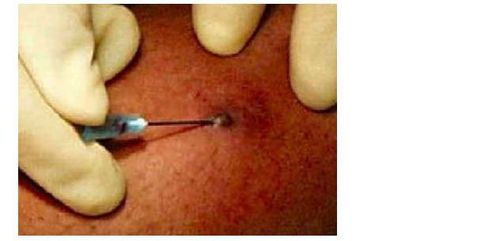
Explain the purpose of the aspiration technique, how to do it, and possible complications (very rare) so that the patient feels comfortable and agrees to cooperate. Exposing the body area to be aspirated, disinfecting the surface skin with alcohol; No need for local anesthesia, except in cases where the tumor is deep and requires aspiration under ultrasound guidance or computed tomography.
4.2 Tools and equipment :
Small needle with diameter ≤ 22G (from 22-27G), length varies from 15mm to 90mm depending on the depth of the tumor. (Figure 2) 10cc thread, gun stock, alcohol sanitizer, cotton ball, tongs, clean slide, gloves, mask.

4.3 Performing aspiration:
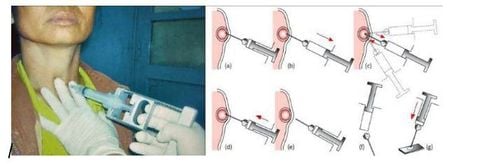
For palpable tumors
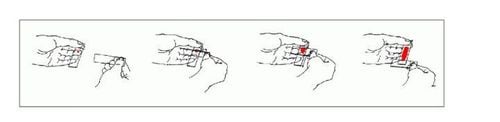
Insert the needle attached sclera to the butt of the gun and hold it with one hand, the other hand immobilize the lesion and tighten the skin surface. Briefly insert the needle perpendicular to the skin surface, entering the lesion (a). Lesions are < 1cm in diameter, the needle puncture site is at the center; lesions >5cm in diameter may have central necrosis, the needle puncture site should be displaced to the periphery; Lesions are 2 - 4cm in diameter, needles should be inserted in 2 positions symmetrically through the center. Pull 2cc piston to create negative pressure (b). Move the needle back and forth about 15-20 times to shred the damaged tissue, when the specimen emerges at the tip of the needle, stop cutting; if still not seen, can change needle direction or increase negative pressure (c). Release the piston to suppress the negative pressure (d). Withdraw the needle from the lesion (e). Remove the needle, pull the piston to draw air into the spool (f). Insert the needle back and push the plunger to spray the specimen onto the slide (g).
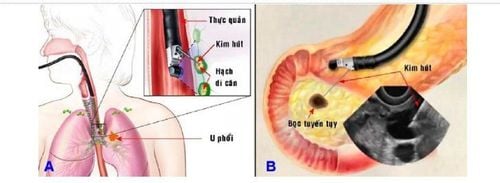
For tumors that are not palpable or deep in the body :
Aspiration is performed under the guidance of ultrasound or computed tomography .
Currently, technological advancements have made it possible to create flexible endoscopes with ultrasound transducers, allowing easy and precise aspiration of lesions only 5mm in diameter, deep in the mediastinum or in the mediastinum. belly; so it is possible to diagnose, classify and determine the extent of cancer spread in order to establish the optimal treatment regimen; Avoid giving the patient an exploratory surgery just for the biopsy.

4.4 Complications :
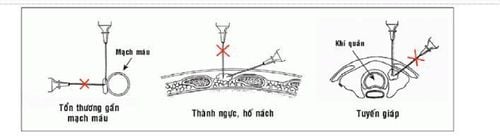
Complications caused by aspiration cytology with a needle less than 22G are generally uncommon, including:
Hematoma at the aspiration site is the most common complication for lesions. superficial with many vascular distribution; This can be easily prevented by asking the patient to keep the cotton in place for about 10 minutes after aspiration.
Infection at the puncture site is rare and can be easily treated with antibiotics.
Pneumothorax and intrapulmonary hemorrhage can occur with aspiration of lesions in the axillary fossa and supraclavicular fossa, and through transthoracic aspiration. Most pneumothorax are of minor degree and are self-resolving. A review of 5,300 cases of transthoracic aspiration cytology showed no fatal events.
Peritonitis, pancreatitis, intestinal perforation may occur after transabdominal aspiration, but are generally rare. The mortality rate due to these events is very low, about 0.006-0.018%.
Currently, the combination with laparoscopic-ultrasound technique allows accurate aspiration of intra-abdominal lesions, helping to limit the above complications.
Dispersion of cancer cells by aspiration has been reported in some cases of transthoracic aspiration, thyroid, pancreas and kidney; however, it is not clear whether this event alters the patient's prognosis for the worse.
Most of the authors agree that the risk of spreading cancer cells by aspiration is real but extremely low (especially when using needles smaller than 22G); therefore does not reduce the diagnostic value or impede the widespread use of fine needle aspiration cytology.
5. Cell smear, fixation and staining:
Specimen sprayed on the slide should be spread thinly in a peripheral blood smear fashion or by applying two slides together and sliding, to form a thin and even layer. (Figure 8)
Cell slides should be properly wet or dry fixed and stained using the May-Grnwald-Giemsa, Diff Quik or Papanicolaou method. Attach the slide and observe under an optical microscope.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: GPB Textbook GPB Department of Medical University Pham Ngoc Thach HCMC.














