This is an automatically translated article.
The article is written by Master, Doctor Hoang Duc Nam - Hepatobiliary Surgery - General Surgery Department - Vinmec International General Hospital.For those tumors that form in the endocrine pancreas, this tumor is usually uncommon and is benign. However, if the tumor begins in the exocrine pancreas, it will most likely be malignant (cancerous).
1. Concepts
The pancreas is an organ of the digestive system, located behind the stomach, across the spine, with endocrine and exocrine functions. In terms of endocrine, although producing hormones that contribute to the regulation of blood sugar... The exocrine function produces enzymes that support the digestion of fats and proteins.Exocrine pancreatic cancer is typically cancer of the ducts that carry pancreatic juice down to the intestines to digest food.

2. Manifestations of pancreatic cancer Most patients with pancreatic cancer present with pain and weight loss, with or without jaundice.
Pain: is a common symptom. Often vague upper abdominal pain, sometimes radiating to the back. Pain is infrequent, initially there is a period of pain relief, sometimes the pain increases after meals. Weight loss : usually due to loss of appetite - feeling bloated despite eating small meals , or diarrhea . Common diarrhea with faeces with fatty scum. Jaundice: the whites of the eyes (sclera) are yellow, then the skin of the whole body is yellow - gradually darkens. Pale stools, losing their usual yellow-brown color; dark brown urine.
Trắc nghiệm: Bạn biết gì về các yếu tố nguy cơ, chẩn đoán và điều trị ung thư tuyến tụy?
Ung thư tuyến tụy phổ biến thứ 10 trong những bệnh ung thư mới và là nguyên nhân thứ 4 gây tử vong do ung thư ở nam, nữ. Bài trắc nghiệm này sẽ kiểm tra kiến thức của bạn về các yếu tố nguy cơ, chẩn đoán và cách điều trị ung thư tuyến tụy.
Bài viết tham khảo nguồn: medicalnewstoday 2019
3. Causes and risk factors Old age: 50% of new cases are over 75 years old, rarely in patients under 40 years old. Overweight, obese. Family history of pancreatic cancer (10%). Smoking: 1 in 3 pancreatic cancer patients smoke. The risk increases fivefold if you smoke more than 30 cigarettes a day. Some medical diseases: Diabetes, chronic pancreatitis, peptic ulcer, gastritis caused by Helicobacter pylori infection. 4. Diagnosis and assessment before treatment Clinical examination: The most common sign is jaundice-itchy skin with many scratches. Abdominal examination is rarely palpable with a small tumor (because the pancreas is located posteriorly). The right subcostal palpation shows a tender mass (gall bladder). In the late stage, there may be large liver metastases, ascites (ascites) or lumpy nodules in the abdominal wall, cervical lymph nodes... Blood tests: bile hyperpigmentation (bilirubin) mainly combined, ALP and GGT ; liver enzymes remained unchanged or only moderately elevated. In most cases, pancreatic enzymes are within normal limits. With pancreatic body-tail tumors, routine blood tests are unchanged. Cancer markers: CA 19-9 is common in bile duct and pancreatic cancers. It can also be increased in colon, stomach, primary liver cancer or in cases of benign biliary obstruction (eg, stones or strictures).

Diagnostic imaging: Abdominal ultrasound: images of intra- and extrahepatic biliary dilatation. Pancreatic tumors over 15mm were detected. It plays an important role in detecting liver metastases, if any. Computed tomography: better than ultrasound in detecting small tumors (>10mm). Assessing the extent of local invasion helps to decide the possibility of radical resection of the tumor. Magnetic resonance: application when the patient cannot have a CT scan. Typical image with pancreatic head mass and biliary dilatation of the pancreatico-bile ducts. Endoscopic cholangiopancreatography: using a gastroscope with a camera and an ultrasound probe, this method is very useful in diagnosing small tumors <3cm. There is a useful advantage in performing ultrasound-guided tumor biopsies. PET CT: detect tumor lesions >10mm. More important than CT scan in detecting distant metastases if present. Endoscopic retrograde cholangiopancreatography (ERCP): often used for catheterization to resolve temporary obstruction rather than for diagnostic purposes.
5. The stages of pancreatic cancer The staging of the disease is to describe the progression and spread of the cancer, thereby deciding the real treatment direction: stage I (earliest) to stage IV - When the tumor has spread to another organ (such as the liver). In general, early-stage cancer has a higher chance of being cured than late-stage cancer.
6. Treatment of Pancreatic Cancer The treatment plan for pancreatic cancer is based on the possibility of complete resection of the tumor. Most pancreatic cancers are diagnosed when there is already extrapancreatic invasion; Only 20% of tumors remain in the pancreas and can be completely resected. Regardless of whether the tumor is resectable or not, the treatment plan of each patient is not exactly the same, usually decided by a panel of oncologists made up of many specialists.
It is possible to combine the following methods to apply the treatment of pancreatic cancer or improve and relieve symptoms of the disease, including:
Surgery Chemotherapy (using drugs) Radiotherapy. Surgery: There are two options depending on the stage of the disease:
Radical surgery: When the tumor is still localized, or just invasive, it can be surgically removed. Total surgical resection of the tumor offers the greatest chance of healing the patient with cancer (required that the remaining resection is free of cancer cells). The most common is a pancreaticoduodenectomy (Whipple surgery). This surgery removes the head of the pancreas, the first part of the small intestine (duodenum), adjacent lymph nodes, the gallbladder, and the distal common bile duct, with or without the distal stomach. After resection, bile, pancreatic juice, and food from the stomach to the small intestine are restored through another loop of the small intestine.
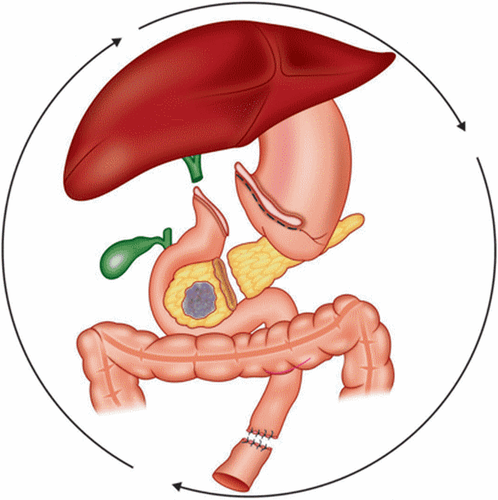
Palliative surgery: In cases where pancreatic cancer has metastasized distantly, or has invaded much of the nearby large blood vessels, it cannot be completely removed. Surgery is sometimes indicated to relieve symptoms and improve quality of life. The most common complications are obstructive jaundice and duodenal obstruction. Interventional measures: Stent insertion: performed through endoscopic retrograde cholangiopancreatitis (ERCP). Advantages of minimal penetration, gentler, quick recovery. Obstacles are possible blockage of stent again, complications of biliary tract infection...
Bile-intestinal junction: creating a channel that directs bile to the intestine to overcome the obstruction. Advantages of effective long-term obstruction resolution than stents, but more severe intervention, need longer recovery time.
Gastro-jejunostomy: With invasive pancreatic head tumor causing duodenal obstruction (first part of small intestine), abdominal bloating, indigestion, vomiting, large gastric obstruction... This surgery helps divert food directly into the intestines through the blocked bowel. Gastrojejunal anastomosis is often combined with biliary-enteric anastomosis (double bypass) to simultaneously resolve two-site strictures.
Chemotherapy: anti-cancer drugs help slow tumor growth, or make it smaller. The drug can be administered orally, or by infusion, and has systemic effects. Depending on the possibility of complete resection of the pancreatic tumor, chemotherapy may be indicated: Before surgery (neo-adjuvant): the aim is to reduce the size and stage of the tumor in order to increase the possibility of radical resection. . After surgery (adjuvant): to destroy and destroy tumor cells that are likely to remain due to the inability to completely remove the tumor. The goal is to reduce the chance of tumor recurrence. Combined with radiation therapy: Sometimes applied to pancreatic tumors with early detection (small, localized). Radiation therapy: Along with the purpose of helping to slow the growth of the tumor, or reduce the size of the tumor. Depending on the accuracy of tumor focus, higher doses of radiation can be applied with less harm to the healthy tissue surrounding the tumor. Dose-modulated radiation therapy. Body positioning radiosurgery. 3D irradiation according to tumor shape. Proton radiation therapy.

7. Possible Problems After Pancreatic Surgery. With the advancement of science and experience, today the surgical mortality rate can be from 5 to 15% compared to nearly 50% in the past. However, even in the best conditions, surgical complications are still a concern, which can be:
Pancreatic fistula: Pancreatic-intestinal fistula from 2-30% depending on technique and experience . Infection: pneumonia caused by lying down for a long time, urinary tract, incision... Bleeding: usually related to the large blood vessels located adjacent to the tumor and the anastomosis. Slow gastric emptying (gastroparesis - related to neurological factors): sluggishness after eating, slow digestion.. Digestive disorders with certain foods such as fat... Loss, weight loss Change in habits Diabetic bowel habit. 8. Palliative care and treatment side effects The goal of cancer treatment is not only to slow down, stop or completely remove the tumor, but also to reduce symptoms and side effects of the treatment. Palliative treatment includes medication, dietary modification, relaxation techniques, psychological support...
9. Treatment results and prognosis Currently, radical resection of pancreatic tumors has achieved many important strides in terms of outcomes and expectations: the average surgical-related mortality <5%, duration average survival is 12-24 months...
10. Post-operative recovery The hospital stay after surgery is about 1-3 weeks. During the hospital stay, the patient may have to wear drains:
Drain the pancreatic juice out (though the surgery and the surgeon's choice). Abdominal drainage: drainage of fluid from the peritoneal cavity. Naso-stomach sonde. The bladder catheter drains urine. Sonde infusion of epidural analgesia in the back. The feeding pump is inserted into the jejunum. In most cases, the drains were removed early after surgery (except for external pancreatic drainage if present) or before hospital discharge. However, there may be cases when it is necessary to bring the drainage home with you when you leave the hospital.
The dietitian will advise before discharge about the post-operative diet. It may be necessary to use additional digestive enzymes to help prevent diarrhea, support food digestion, regulate blood sugar... The use of this support product may be temporary after surgery, or must be used for life depending on the progress. .

Take care of yourself at home:
Eat small, easily digestible meals. Use insulin, digestive enzyme supplements as indicated. Walk as much as possible. Do not carry heavy objects. Do not drive if self-administering narcotic pain medication. Prevent constipation by drinking plenty of fluids and taking laxatives if needed. Customers who need medical examination and treatment at Vinmec International General Hospital can directly visit facilities nationwide, or contact the hotline HERE.