This is an automatically translated article.
The article was written by Dr. Nguyen Manh Ha - Department of Radiation Therapy - Vinmec Times City International HospitalCervical cancer is the fourth most common cancer in women worldwide, with an estimated 5,300,000 new cases each year resulting in 7.5% of all cancer deaths among women. About 85% of deaths occur in developing countries from cervical cancer every year. The high global mortality from cervical cancer [1] (~52%) can be reduced by effective screening and treatment programmes.
Advances in radiotherapy technology have greatly helped in curing cancer patients by delivering sufficient doses to the tumor and minimizing the dose to surrounding vital structures [2] .
In 3-D compatible radiotherapy techniques (3DCRT-3Dimension Conformal Radiotherapy), people find that with front-to-back (0 degrees)/anterior (180 degrees) projection fields or plans made up of 4 boxy fields ( 0.90,180,270 degrees) delivers unnecessary doses to nearby vital organs, thus leading to complex treatment-related complications after cure or disease recurrence.
Conventional techniques have given way to intensity-modulated radiotherapy (IMRT) over the past two decades and most recently, we have seen the emergence of volume-modulated radiotherapy. VMAT (Volume Modulated Arc Therapy).
IMRT offers the advantage of dose modulation to deliver a dose large enough to treat volume while limiting those high doses to surrounding organs. However, the amount of MU (monitor unit) emitted by this technique is very large compared with conventional techniques that increase the risk of a secondary cancer [3,4] known as radiation malignancy. VMAT can overcome these disadvantages of IMRT and promote the superior advantage of dose delivery by using a partial or full arc that can produce a smaller number of MUs in a shorter treatment time. [5]. To evaluate how the dose distribution from VMAT plans is affected by the number of arcs and radiant energy used we conducted the study: “Evaluating the effect of energy levels and numbers arc volume to dose distribution in arc volume-modulating radiotherapy for cervical cancer”.
Trắc nghiệm về virus HPV
Hiện nay, những căn bệnh liên quan đến HPV ngày càng trở nên phổ biến và được cảnh báo nhiều hơn trên các phương tiện truyền thông. Hiểu đúng về HPV sẽ giúp bạn tránh được không ít nguy cơ dẫn đến ung thư các bộ phận sinh dục.
Bài dịch từ: webmd.com
1. Objects and research methods
1.1 Subjects From October 2018 to May 2020, 15 cervical carcinoma patients received radiation therapy at the Department of Radiation Therapy - Vinmec Times City International General Hospital. Among 15 patients, the mean age was 43.5±5.9.
Of which, there are 07 stage (III) patients and 08 stage (II) patients according to the stage classification of NCCN (2019). VMAT plans with 6 MV and 15 MV energies using one arc (SA-Single Arc), two arcs (DA- Dual Arc) and three arcs (TA-Triple Arc) were developed for each patient.
1.2 Research method 1.2.1 Research procedure All patients (patients) were immobilized by using a mask with subframe log (Civco, USA) to ensure that the part from abdomen to femur was remain stationary and stable throughout the course of radiation therapy.
Computed tomography (CT) images with a thickness of 2.5 mm were obtained on a 16-slice CT simulation machine GE optimal 580 (GE, USA). The patient was instructed and performed the bladder preparation procedure before the CT simulation and treatment.
Accordingly, the patient will empty the bladder and drink a certain amount of water 500-1000ml depending on the patient, then wait for a fixed period of 45 minutes or more to make sure the bladder is full. fill.
An experienced radiologist that accurately identifies the risk organ areas (Ogan at Risk (OAR) for all patients, together with a physical engineer can design the dose calculation for the radiotherapy plan. OAR includes: bladder (Bladder), rectum (rectum), bowel bag (bowel bag), bilateral femoral head (Femur_Lt, RT), spinal cord (Spinal Cord), pelvis (Illiac bone), tissue part normal (Body-PTV).
PTV was determined based on guidelines recommended by the International Commission on Radiation and ICRU Units 50 and ICRU 62 [6,7] and the RTOG cancer radiotherapy protocols (Lim et al., 2011). . PTV was assigned a dose of 50.4Gy/28 fractions and gave the patient one dose per day, 5 fractions per week.
All VMAT plans (SA6MV, DA6MV, TA6MV, SA15MV, DA15MV, TA15MV) are calibrated for normalization or normalization to the same standard so that the comparison is as accurate as follows: 100% of the indicated dose (70Gy) covers up to 95% of the target volume.
Regarding OAR: The dose to critical organs should be minimized to the maximum extent reasonable in Table 1 and should not affect the treatment goal.

1.2.2 VMAT plan The VMAT plans (SA, DA, TA) for each patient are set up by us on Eclipse planning software version 13.0 of Varian (USA). The plans use coplanar gantry arcs, use 6 MV energy, 600 MU/min dose rate, AAA algorithm for optimization calculation.
Plan SA includes a gantry arc designed to rotate from 179 degrees to 181 degrees. The DA plan includes a gantry arc designed to rotate from 179 degrees to 181 degrees (counterclockwise) and a counter-arc (clockwise) with two collimator angles of 10 and 80 degrees, based on previous research our group about the effect of collimator angle on dose distribution in the VMAT plan [8].
The TA plan is similarly designed, including 1 gantry arc rotated from 179 to 181 degrees with a 10 degree collimator angle and the other 2 arcs with the same 80 degree collimator angle, a gantry angle from 179 to 181 degrees and vice versa with the reason is that the large length PTV volume can divide an arc into two arcs with a smaller projected field size to reduce the displacement distance between the MLC leaves and reduce the error between the MLC leaves. The SA, DA, and TA plans were then set at 15MV per patient, the same design parameters as for 6MV.
1.2.3 Plan evaluation and comparison The plan quality index of VMAT plans was analyzed using a dose-volumetric (DVH) plot. The DVH plot represents all dose information in a two-dimensional curve and is referenced based on the guidelines of the International Commission on Radiation Units (ICRU83) [9].
Coverage of planned volume (PTV) and mean dose to organs of risk (OAR) mean (Dmean) and maximum dose (Dmax), index of conformity (CI) [10 ] and the homogeneity index (HI) were analyzed for all plans. For all patients, the total number of MUs per fraction and the duration of exposure for each plan were compared.
Conformity index (CI) is defined as follows: CI = TVRI/TV Where: TVRI = target volume covered by reference dose (volume of PTV receiving reference dose in the report is 98%) . TV = target volume. The ideal value is 1. The Concordance Index (CI) represents how well the iso-dose curve matches the shape and size of the target.
The homogeneity index (HI) is defined as follows: HI = (D2% - D98%)/D50% Where: D2% is dose up to 2% of PTV volume; D98% is dose up to 98% of PTV volume; D50% is dose up to 50% of PTV volume. The homogeneity index (HI) describes the uniformity of dose within a target volume and is calculated directly from the dose-volume chart statistics. The closer the HI index is to zero, the better (ICRU83).
1.2.4 Statistical analysis Statistical comparison of PTV and OAR dose coverage among VMAT plans was performed using statistical data analysis using the SPSS v15.5 system. Results are reported as mean and standard deviation. Statistical significance values are kept at p < 0.05, p values > 0.05 are not significant (NS-nonsignificant).
2. Actual results


All evaluated plans met the requirements for limiting dose and dose distribution to PTV, eligible for clinical treatment economy before being compared. Dose coverage to PTV was compared across all energy levels and arc numbers (table 2).
V98 volume for plan TA6MV(97.93±0.35) is better than DA6MV(97.84±0.34), SA6MV(97.63±0.23); TA15MV(97.98±0.39) plan is better than DA15MV(97.87±0.34), SA15MV(97.68±0.3) (p < 0.05).
Doses up to 2% (D2) of PTV in the SA6MV(56.31±1.27) and SA15MV(56.07±1.42) plans were the largest (p<0.05). The TA6MV plan had a better CI (0.979), HI (0.112) than the CI (0.978) and HI (0.117) for DA6MV and SA6MV (CI=0.976; HI=0.132), similar to CI (0.979), HI (0.111) for DA6MV and SA6MV. with TA15MV better than DA15MV (CI=0.978; HI=0.117) and SA15MV(CI=0.976; HI=0.127), p<0.05.
Figure 1 clearly shows the dose distribution of V98, D2, CI, HI to PTV between the TA6MV and TA15MV plans; DA6MV and DA15MV were not significantly different (p>0.05).




Table 2 results in less dosing time and number of MUs in SA plans than in DA and TA plans at both 6MV and 15MV energy levels (p<0.05).
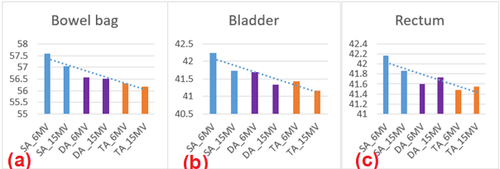
The evaluated parameters showed a significant reduction in OAR dose (table 3). Mean dose (Dmean) and maximum dose (Dmax), the volume received 40Gy dose (V40Gy) to the bowel bag (Bowel bag) of the TA plan was better than that of the SA, DA plans at both energy levels. 6MV and 15MV (p<0.05).
Mean bladder dose was also better in TA plans than in SA and DA plans at both 6MV and 15MV (p<0.05). At 6MV, the mean rectal dose in TA6MV(41.48±3.22) plans was better than DA6MV(41.66±3.22), SA6MV(42.17±3.11) (p<0.05).
Dose to healthy tissue volume (Body-PTV) did not show much difference between plans in the same 6MV (SA, DA, TA) or 15 MV (SA, DA, TA) energy levels (p>0.05) ); When comparing the energy levels, TA15MV and DA15MV have lower doses of Dmean (9.3; 9.5), V5Gy (46.68; 46.64) than Dmean (10.2; 10.0), V5Gy (47.2; 47.0) of TA6MV and DA6MV (p<0.05).



3. Discussion
The results in Table 2 and Figure 1 show that TA plans have better dose distribution to PTV than SA, DA at both 6MV and 15MV energy levels (p<0.05). The results are explained because TA uses 3 arcs more than SA (1 arc) and DA (2 arcs), so the ability to adjust dosage and optimize is better than other plans. Comparison of the effect of energy levels on the DA6MV with DA15MV and TA6MV with TA15MV plans (Figure 1) showed that the results were not significantly different (p>0.05), which was similar to the results of Sternick et al. [11] in the study of the effects of 4-18MV energy in prostate IMRT.
Our report also gave similar results with author Lalit Kumar [12] in comparing the effects of 6, 10, 15MV levels in cervical cancer and author Girigesh Yadav [13] when comparing images Effect of 6, 10, 15MV in SA, DA plans for uterine cancer.
At the same time Because the number of MU emitted from 1 arc is also smaller than the multi-sector plans. This result is similar to the study of Lalit Kumar [12] on the number of MUs. On the other hand, the number of MUs in TA15MV is less than in TA6MV because the 15MV energy level has a greater percent depth than 6MV, so the number of MUs emitted to achieve the required dose at the same depth of 15MV is less. The number of MUs is better represented by the graph in Figure 3c.
Table 3 and Figure 2 show that the dose to critical organs such as: Dmean, Dmax and V40Gy to the Bowel Pouch and Dmean to the bladder, Dmean to the rectum of the TA plan is better than that of the SA plans, DA at both 6MV and 15MV energy levels (p<0.05) is explained as the better modulation ability in TA plan thanks to the large number of arcs, so the number of modulation points is larger.
Dose to healthy tissue volume (table 2, figure 3a) when comparing energy levels in TA and DA plans, the Dmean, V5Gy dose of 15MV was superior to 6MV (p<0.05), which was explained as Due to the larger number of MUs in the MU plans, the low dose fraction around the PTV volume would be larger, which is consistent with the studies presented [14,15].

Table 4 and Figure 3b show that the values of Dmean, Dmax to the pelvis in TA plan are better than DA and SA at both 6MV and 15MV (p<0.05). At 15MV energy the dose of V10Gy in the TA15MV plan (93.01±4.11, p<0.05) was lower than in the other plans.
At 6M the dose of V40Gy in the TA6MV plan (15.4±5.35) was the lowest (p<0.05). The V10Gy in the TA15MV plan was better, and the V40Gy in the TA6MV the lowest, explained in the same way as above because of the greater percent depth 15MV energy level with 6MV requiring less MU to deliver the dose to the same depth so the dose fraction The high dose was more concentrated near the PTV (V40Gy) while the low dose V10Gy part around the PTV was less than the 6MV level.
4. Conclusion
The study found that 15MV high-energy plans were no better than 6MV in dose distribution to PTV and to critical organs. The TA6MV plan is a good choice for the treatment of cervical cancer because of its higher dose coverage, homogeneity, and relevance to the treatment target, and better protection of critical organs.References:
[1] . World Health Organization (WHO) Reports on Cervical Cancers. HPV and Cervical Cancer in the World 2007, vol. 25(Suppl. 1). 2007. [2] . Gupta D, Shukla P et al. Comparitive study of efficacy, tolerability of four field box technique vs. two field anterior posterior technique in locally advanced carcinoma cervix. Cancer Biol Ther 2009. [3] . Kry SF, Salehpour M, et al. The calculated risk of fatal secondary malignancies from IMRT. Int J Radiat Oncol Biol Phys2005. [4] . Kry, Kry SF, Followill D, et al. Uncertainty of calculated risk estimates for secondary malignancies after radiotherapy. Int J Radiat Oncol Biol Phys 2007. [5] . Cozzi L, et al. A treatment planning study comparing volumetric arc modulation with RapidArc and fixed field IMRT for cervix uteri radiotherapy. Radiother Oncol2008.
[6] . ICRU Report 50. Prescribing, Recording, and Reporting Photon Beam Therapy (1993). [7] ICRU Report 62. Prescribing, Recording, and Reporting Photon Beam Therapy (1999).
[8] . Nguyen Dinh Long, Tran Ba Bach et al.: Effect of Collimator angle on dose distribution in arc radiation therapy for NPC, VN Journal of Oncology No. 5 (2017).
[9] ICRU Report 83. Prescribing, Recording, and Reporting Photon-Beam IMRT (2010).
[ten] . Van't Riet A, (1997): A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation. Int J Radiat Oncol Biol Phys, 37, 731-6. [11] . Sternick ES, et al. IMRT: What photon energy isbest? Medical Physics; 1997. p. 418-9.
[twelfth] . Lalit Kumar et al. The dosimetric impact of different photon beam energy on RapidArc radiotherapy planning for cervix carcinoma, Journal of Medical Physics (2015).
[13] . Girigesh Yadav el at. Dosimetric influence of photon beam energy and number of arcs on VMAT in carcinoma cervix: A planning study, Published by Elsevier (2016).
[14] D'Souza WD, Rosen II. Nontumor integral dose variation in conventional radiotherapy treatment planning, Med Phys 2003.
[15] . Pirzkall A, et al. The effect of beam energy and number of fields on photon-based IMRT for deep-seated targets. Int J Radiat Oncol Biol Phys 2002.













