This is an automatically translated article.
The article is expertly consulted by Master, Doctor Ton That Quang - Head of Anesthesia - Anesthesia Unit - Department of General Surgery - Vinmec Nha Trang International General Hospital.1. What is a small pelvic tumor surgery?
The female pelvis is located below the terminal crest of the pelvis and includes the uterus, appendages, bladder, and rectum.Subframe tumors are tumors that develop from components in the subframe such as ovarian tumours, uterine tumours... Indications for surgical resection of subframe tumors include ovarian subsquamous tumours. causing ovarian adhesions, large uterine tumors or suspected cases of pelvic malignancy. When surgery, if the tumor is difficult to remove, there will be an indication of hysterectomy or oophorectomy to completely remove the tumor.
Surgery to remove tumors in the pelvic region can be laparoscopic or open surgery, laparoscopic surgery is indicated in most cases due to its superiority compared to open surgery. However, there are also some cases with contraindications to laparoscopic surgery requiring open surgery.
2. Endotracheal anesthesia in tubal resection surgery
Endotracheal anesthesia for tubal resection is a method of general anesthesia with endotracheal intubation with the aim of helping to control breathing during surgery and resuscitation after surgery.
3. Endotracheal anesthesia procedure
3.1 Preparation Performer: Doctor, nurse in anesthesiology and resuscitation department. Technical means: Anesthesia machine system with ventilator; balloon oxygen source; monitor vital functions including electrocardiogram, arterial blood pressure, SpO2, EtCO2, temperature, breathing rate; defibrillator, phlegm aspirator. Laryngoscope, endotracheal tube of different sizes, suction tube, mask, squeeze balloon, oropharyngeal cannula, Magill pliers, soft mandrin. Medicines: Prepare drugs used in anesthesia resuscitation and handling of accidents. Other means of precaution in case of difficult intubation: Cook tube, laryngeal mask, flexible bronchoscope, mouth opener, tracheostomy kit... Patient: Full pre-anesthesia examination , detect and prevent the risk of accidents that may occur. Counseling and explaining about possible complications during anesthesia and pelvic tumor resection. Risk assessment of cases at risk of difficult intubation. Use sedation the night before surgery if needed.
Patient position: Lie on back, breathe 100% oxygen 3-6 l/min at least 5 minutes before induction of anesthesia. Install a monitor to monitor vital signs, if patients undergoing laparoscopic surgery must have EtCO2 parameters. Establish an effective infusion and administer pharmacological pre-anesthesia. Anesthesia:
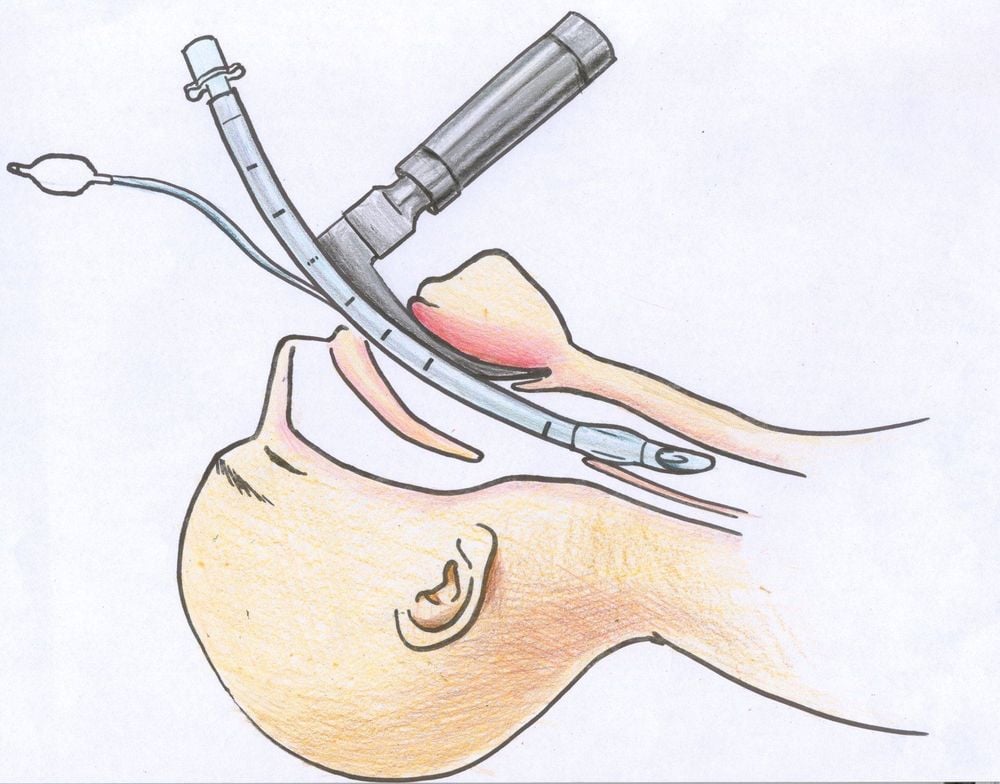
Anesthesia can be initiated by intravenous anesthetic (propofol, etomidate, thiopental, ketamine...), inhalation or a combination of the two. Combine some drugs to increase the effect of anesthetics such as: opioid pain relievers (morphine, fentanyl..), muscle relaxants if necessary. Oral intubation : The condition for intubation is when the patient is in deep sleep, the degree of muscle relaxation is sufficient (in most cases).
Open the patient's mouth, place one hand under the neck to help straighten the neck, then insert the laryngoscope to the right of the mouth, push the patient's tongue to the left, push the lamp deeply, coordinate with the right hand to press the cricoid cartilage downward and Find the epiglottis, the glottis. Perform rapid induction of anesthesia and the Sellick maneuver in cases of full stomach. Pass the endotracheal tube through the glottis gently, stopping when the balloon of the endotracheal tube passes about 2-3 cm across the vocal cords. Remove the laryngoscope and inflate the endotracheal balloon. Check that the endotracheal tube is in the correct position by listening to the lungs and EtCO2 results. Secure the tube with tape and place the canul in the mouth to prevent biting the tube (if necessary). In cases of difficult intubation, a difficult intubation procedure should be used. Maintenance of anesthesia: Maintain anesthesia with intravenous or inhalation anesthetics, analgesics, and muscle relaxants (if needed).
Monitoring:
Need to control breathing with a ventilator or hand-held oxygen source. Monitoring the depth of anesthesia based on heart rate, arterial blood pressure, sweating, tearing... Monitor signs and prevent cases of endotracheal intubation in the wrong position, folding...
The patient is awake and follows orders; Lift head for more than 5 seconds, TOF >0.9 (if any); Spontaneous breathing, breathing rate within normal limits; Stable pulse and blood pressure; Body temperature > 35 degrees Celsius; There were no complications from anesthesia and after surgery.
4. Complications and management of complications due to intubation
4.1 Reflux of gastric juice into airway Signs: There is digestive fluid in the oral cavity and airways. Treatment: Drain the fluid, place the patient in a low lying position, tilt the head to one side; Rapid intubation of the endotracheal tube and aspiration of the airway fluid; Monitoring and prevention of lung infections after surgery. 4.2 Hemodynamic disorders Hypotension or hypertension, arrhythmia (may be bradycardia, tachycardia, arrhythmia). Treatment depends on the signs and causes.
Treatment: Need to ensure immediate pulmonary ventilation and provide 100% oxygen, solve the cause.
4.5 Complications after extubation After extubation, the patient may experience a number of complications such as: respiratory failure, sore throat hoarseness, spasms of the larynx, trachea and bronchi, upper respiratory tract infection, laryngitis, trachea.
Depending on each case and each cause, the doctor will offer an appropriate treatment method.

Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Master. Dr. Ton That Quang has more than 15 years of experience working in the Anesthesia - Resuscitation industry. Doctor Quang was a doctor at the Department of Anesthesiology and Resuscitation at Khanh Hoa General Hospital and a lecturer at the provincial level of Emergency Resuscitation in Obstetrics and Gynecology before being an Anesthesiologist and Resuscitation Doctor at the Department of General Surgery, General Hospital. International Vinmec Nha Trang.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.