This is an automatically translated article.
This article is expertly consulted by Master, Doctor Nguyen Le Duc Hoang - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.Diabetic hyperosmolar coma is a serious diabetic complication that can be life-threatening. Therefore, it is necessary to give first aid immediately when the patient encounters this complication and the emergency procedure should be performed according to the standard protocol.
1. Overview of diabetic coma
1.1 What is Diabetic Hyperosmolar Coma? Hyperosmolar coma is an acute, life-threatening complication of diabetes mellitus. The disease is common in patients over 65 years old, with type 2 diabetes, more common in women than in men, accompanied by diseases that reduce the ability to drink water. The disease has a poor prognosis with a high mortality rate (40 - 50%) even when receiving emergency care at medical facilities with modern equipment. If the patient survives, it is also easy to live with sequelae.Pathogenesis: In patients with diabetes, insulin deficiency causes an increase in glycogen breakdown in the liver, increased gluconeogenesis, and a decrease in the use of glucose by the tissues, leading to an increase in blood glucose levels. With hyperglycemia, the patient will increase diuresis due to osmosis and consequent dehydration. More water loss than salt loss will increase blood osmotic pressure. When the osmotic pressure rises above 320 mOsm/kg, water from the interstitial spaces and in the cells (including CNS cells) is pulled into the lumen, causing coma and dehydration. Often, when symptoms of consciousness disorder are present, water loss can account for up to 25% of body weight.
1.2 Causes of disease Factors that increase the risk of diabetic coma include:
Infection: The most common cause, accounting for 57.1%. Common bacterial infections are pneumonia, urinary tract infections and bacteremia; Diabetes is not detected, the patient is comatose due to increased osmotic pressure because the early symptoms of diabetes are not recognized; The patient does not comply with the diabetes treatment regimen; Having comorbidities such as: cerebrovascular accident, mesenteric thrombosis, acute myocardial infarction, increased or decreased body temperature,... Using diuretics, corticosteroids or drinking alcohol.

Sử dụng một số loại thuốc có nguy cơ cao
Consciousness disorders of varying degrees, from lethargy to deep coma; Aphasia, hemiplegia, nystagmus,...; Signs of severe dehydration: Dry skin, very dry oral mucosa, collapsed neck veins, rapid pulse, little urine, low blood pressure, rapid weight loss, increased body temperature,...; Clinical manifestations of risk factors for disease: Infection, myocardial infarction, cerebrovascular accident,... Subclinical tests:
Increased blood sugar over 40mmol/l; Blood osmolality above 320 mOsm/l; Arterial blood gas: pH above 7.3, bicarbonate above 15 mmol/l; No or very little ketones in urine ; Blood sodium usually rises above 145 mmol/l. *Note: A differential diagnosis of hyperosmolar coma is required from diabetic ketoacidosis.
Diagnosis of risk factors for disease
Infections: Including pneumonia, urinary tract infections,...; Heart attack; Stroke; Big stress; Mistakes in disease treatment: Overuse of diuretics, corticosteroids, mannitol.

Xét nghiệm máu giúp chẩn đoán bệnh
2. First aid for comatose patients with increased osmotic pressure due to diabetes
2.1 Principles of first aid First aid; Quick and complete translational compensation; Adjust electrolytes; Use insulin to control blood sugar; Diagnosis and treatment of risk factors for increased osmotic pressure such as urinary tract infections, pneumonia,... 2.2 Initial management and emergency transport Ensure the patient's breathing and circulation during transport Emergency transfer, rapid early replacement of intravenous fluids on site and during transportation.2.3 Hospital emergency Resuscitation
Immediately place a large intravenous line, then insert a central venous catheter to rehydrate if possible; Start infusion of 1 liter of 0.9% sodium chloride in 1 hour, in 2 hours according to an estimate of 8-10 liters of water shortage; During fluid resuscitation, it is necessary to closely monitor the patient's pulse, blood pressure, urine, and oxygen saturation; In case of severe volume depletion causing hypotension, sodium chloride 0.9% 1 liter/hour should be infused until the hypotensive state stops; If the patient is mildly dehydrated, adjust the sodium accordingly according to the doctor's prescription and standard treatment regimen. Using insulin
The use of insulin in small doses is indicated early:
Monitor capillary blood sugar every 1 hour for the first 3 hours, then every 3 hours to adjust the insulin dose for the patient; Use insulin 0.1 units/kg, intravenously followed by continuous intravenous infusion of 0.1 units/kg/hour; If blood glucose does not fall by 3 mmol/l in the first hour, the insulin dose can be doubled; When blood glucose reaches 15 - 16 mmol/l, reduce insulin to 0.02 - 0.05 units/kg/hour; Ensure blood glucose at 11 - 15 mmol/l until the patient regains consciousness.

Truyền insulin theo đường tĩnh mạch
After insulin injection, potassium must be given immediately because hypokalemia in a coma increases osmotic pressure, especially after insulin is very dangerous and can cause death:
Monitor electrolytes 6 every hour until the patient is stable; If kidney function is normal, urine output is 50ml/hour or more; If serum potassium is less than 3.5 mmol/l, insulin and intravenous infusion of 1 - 2 g/hour (equivalent to 20 - 30 mmol potassium/hour) should be used until the serum potassium level is above 3.5 mmol/l; If the initial potassium concentration fluctuates at 3.5 - 5.3 mmol/l, add Potassium 20 - 30 mmol/l of the intravenous fluid to ensure that the blood potassium concentration remains at 4-5 mmol/l; If the initial potassium concentration is above 5 mmol/l, do not perform potassium replacement but check the serum potassium every 2 hours. When the patient is stable and able to eat, switch to subcutaneous insulin. Continue IV insulin infusion 1-2 hours after subcutaneous insulin injection to ensure adequate insulin concentration in the patient's blood. Anticoagulation
Patients in a diabetic coma with high osmotic pressure are at high risk of embolism, so it is imperative to use anticoagulants in all cases (if there are no contraindications).
Treat the associated cause
Use antibiotics if there is evidence of infection; Treat the cause of hyperosmolar coma to prevent recurrent coma; Use medications to prevent deep vein thrombosis. 2.4 Monitoring during treatment Monitor blood sugar every 1 hour; Monitor blood electrolytes every 3 - 6 hours; Continuous ECG on monitor or record every 3 - 6 hours; Monitor blood urea and creatinine to assess functional renal failure.
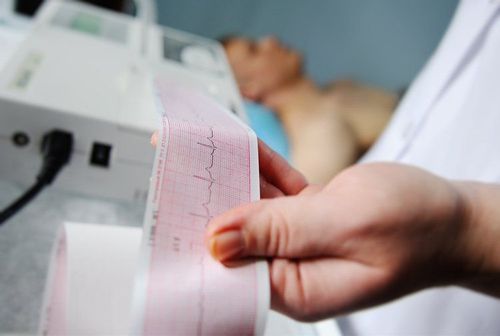
Theo dõi điện tim của bệnh nhân
3. Complications of emergency diabetic coma
Complications due to not treating the disease properly are vascular occlusion (messenteric embolism, myocardial infarction,...) and rhabdomyolysis; Rapid rehydration can lead to cerebral edema in children and respiratory failure in adults. Although a rare complication, cerebral edema can be fatal in children. Symptoms of cerebral edema are headache, sudden change in consciousness or loss of consciousness, bradycardia, papilledema, and increased blood pressure. Gradual treatment of raised osmotic pressure can avoid complications of cerebral edema in children. At the same time, it is possible to treat with mannitol and dexamethasone as prescribed by the doctor.4. How to prevent diabetic coma?
Patients with diabetes need to be monitored for disease progression, altered consciousness, and closely monitored blood sugar; Diabetics should be guided to maintain a reasonable diet and use insulin exactly as prescribed by the doctor; Patients need to be examined, detected and treated for comorbidities such as cardiovascular diseases, infections, etc. Diabetic hyperosmotic coma is very dangerous, has a high mortality rate if not detected early. Therefore, when there are signs of illness, family members need to immediately take the patient to the hospital and strictly follow the treatment regimen of a specialist to avoid serious complications.Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Doctor Nguyen Le Duc Hoang has a lot of experience in the treatment of Resuscitation - Adult Emergency. Dr. Hoang used to work at the Intensive Care Unit at C Hospital in Da Nang before working at Vinmec Danang International General Hospital as it is today.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
MORE:
What type of diabetes requires insulin? When do diabetics inject insulin? What should be noted in the treatment of dyslipidemia in diabetics?














