This is an automatically translated article.
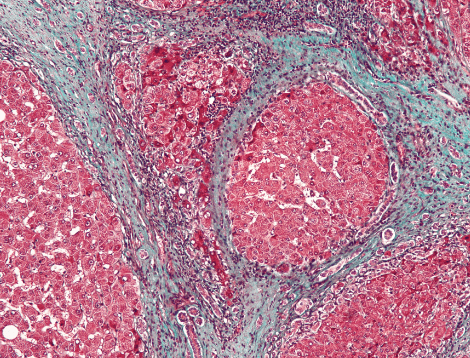
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalDetermining the efficacy and safety of anti-cirrhotic drugs for cholestatic liver disease remains a challenge because there are different modalities available to assess liver fibrosis in patients.
1. Primary cholangitis and primary sclerosing cholangitis
Despite decades of use and recent drug development, UDCA remains the standard of care for primary cholangitis (PBC). UDCA is a hydrophilic bile acid that has been shown to improve liver biochemistry and slow down histological progression of disease, improving liver transplant-free survival.In a study performed by Corpechot et al., UDCA therapy was shown to significantly reduce the rate of progression from early-stage disease to extensive cirrhosis or cirrhosis at a rate of 7% per year. year for UDCA compared with 34% for placebo (P < 0.002).

2. The Role of Norursodeoxycholic Acid
Norursodeoxycholic acid is a C23 homolog of UDCA that showed in a randomized, phase 2, placebo-controlled study, significant biochemical improvements including reductions in alkaline phosphatase (ALP) and liver enzymes. However, further studies are required to evaluate histological efficacy. Unlike its frontline role in PBC, UDCA has questionable roles in the treatment of primary sclerosing cholangitis (PSC). The AASLD recommends against the use of UDCA due to the lack of beneficial data and the potential for worse outcomes.3. The role of obeticholic acid
Second-line treatment options, including obeticholic acid for UDCA nonresponders, have shown some promising non-histological results. Its approval was based on the POISE study, a 1-year, placebo-controlled study that demonstrated significant reductions in ALP, total bilirubin, and aminotransferases. Investigators also assessed underlying liver disease by noninvasive measures such as TE and enhanced cirrhosis scoring, but the results did not differ significantly between the OCA and placebo groups.It should be noted that patients taking OCA, experienced a dose-dependent increase in itching compared with placebo. The POISE Biopsy Facility evaluated histological results when comparing paired liver biopsies before and after 3 years of OCA treatment in PBC patients receiving concomitant UDCA. The results showed a statistically significant improvement or stabilization of fibrosis (71% of patients), a decrease in collagen area ratio (-31%, P = 0.013), and a density of collagen fibers (-35%, P = 0.021), collagen mesh index (-7%, P = 0.008) and fibrosis composite score (-25%, P = 0.002).
Currently, OCA is being investigated in a phase 4 study (COBALT; NCT02308111) evaluating clinical outcomes, including noninvasive liver scores and liver biopsy specimens that may further support clinical outcomes encouraging in PBC patients. Regarding the role of OCA in PSC treatment, the AESOP trial demonstrated biochemical improvement, however histological data were not collected.
4. The role of the drug bezafibrate
Third-line options for the treatment of PBC include bezafibrate, and its efficacy and safety were first demonstrated in a phase 3 placebo-controlled trial (BEZURSO; NCT01654731). Participants were assigned to receive bezafibrate or placebo in addition to UDCA for 24 months. Results included normalization of ALP and aminotransferase in the bezafibrate group compared with placebo. This included a 15% reduction in liver stiffness and a reduction in enhanced liver fibrosis scores in the treatment group compared with placebo. A subgroup of patients had histological data before and after the study, and changes in histological stage, fibrosis stage, and activity level were not significantly different between the two groups. Significant adverse events included a baseline 5% increase in serum creatinine compared with a 3% decrease in the placebo group. Myalgias were also more common in the treatment group, but this was not statistically significant.In summary, there are countless drugs that have been and continue to be tested in both PBC and PSC. However, many drugs have been shown to be ineffective in the treatment of cholestatic liver disease. Studies have mainly investigated the biochemical effects of the drug, and there are limited studies evaluating progression and/or regression of liver fibrosis.

5. The role of Phlebotomy in cirrhosis caused by iron overload
Excess accumulation of iron is toxic to hepatocytes because it allows the generation of excessive reactive oxygen species leading to cell damage and secretion of pro-fibrinolytic cytokines. The fiber response is mediated not only by oxygen species, but also by a large array of iron-induced cellular signaling pathways, HSC activation by iron-associated proteins, and possibly iron-mediated ECM regeneration. Phlebotomy is a commonly used treatment for inherited hemoglobinopathy, as it not only removes excess iron in the body, but also promotes hematopoiesis using systemic iron stores.In a study conducted by Falize et al., 69% of participants with stage F3 and 35% with stage F4 had fibrosis demonstrated regression of fibrosis after ablation (minimum reduction in fibrosis). 2 METAVIR units). In people who cannot have varicose veins surgically, chelating agents have been shown to be effective in removing excess iron from the liver and ultimately contributing to the control of fibrosis. The benefit of chelation was also demonstrated by Deugnier et al., who performed a study evaluating the effectiveness of deferasirox in people with beta thalassemia. Results showed stabilization of the Ishak fibrosis staging score or improvement (change 2) in 82.6% of patients, and an improvement in the mean Ishak necrotizing inflammation score with a mean value of -1.3 (P < 0.001) in those treated for at least 3 years.
In conclusion, determining drug efficacy remains a challenge because there are different modalities available to assess liver fibrosis, which are far different from traditional liver biopsies. As seen in this review, there are a multitude of clinical trials from observational and therapeutic studies. In the authors' opinion, future studies are required to standardize clinical and fibrosis criteria to allow a better understanding of drug efficacy as a single drug or in combination. together. While most trials currently focus on MAFLD, further research is needed among all causes of cirrhosis to improve benefit worldwide.
To protect everyone's health, now, Vinmec International General Hospital provides customers with standard to advanced hepatobiliary screening packages to help diagnose cirrhosis in particular and hepatobiliary diseases. Generally speaking.
Vinmec is the leading prestigious and reliable address in the field of screening and treatment of hepatobiliary diseases, with the following outstanding advantages:
As one of the few hospitals across the country applying ultrasound Liver tissue recovery (also known as ARFI technique) to monitor liver disease, assess the degree of cirrhosis such as imaging, test kits from basic to advanced. With the state-of-the-art LOGIQ E9 ultrasound system, a powerful and flexible ultrasound imaging system that meets a wide range of general examination needs. New technology using Shear Wave: This is a technology that allows qualitative and quantitative measurement of the elastic energy of the parenchyma through a color-coded table along with the value of elastic levels in Kpa pressure units. A team of specialists and specialists with extensive experience and expertise helps the treatment process to be highly effective, shortening the treatment time. Professional, comprehensive examination and consultation service, civilized, polite, safe and sterilized medical examination space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferenceToosi AE. Liver Fibrosis: Causes and Methods of Assessment, A Review. Rom J Intern Med. 2015;53:304-314. [PubMed] [DOI] Hernandez-Gea V, Friedman SL. Pathogenesis of liver fibrosis. Annu Rev Pathol. 2011;6:425-456. [PubMed] [DOI] Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol. 2017;23:8263-8276. [PubMed] [DOI] Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24:908-922. [PubMed] [ DOI ] Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: Final Data for 2017. Natl Vital Stat Rep. 2019;68:1-77. [PubMed] Konstantinos Damiris, Efficacy and safety of anti-hepatic fibrosis drugs, World J Gastroenterol. Nov 7, 2020; 26(41): 6304-6321