This is an automatically translated article.
The article was written by Master, Doctor Ha Thi Thu Hien - Pathologist - Laboratory Department - Vinmec Times City International Hospital1. Can cervical cancer be detected early?
The best way to detect cervical cancer early is to have regular screening tests. Tests to screen for cervical cancer include the HPV test and the cervical smear test (Pap smear and liquid-based cytology). These tests can be done alone or at the same time.
Early detection greatly improves the chances of successful treatment of precancerous and cancerous diseases. Being aware of any signs and symptoms of cervical cancer can also help avoid delays in diagnosis.
As recommended by the American Cancer Society for the Prevention and Early Detection of Cervical Cancer
The American Cancer Society recommends that women follow these guidelines for early detection of cervical cancer. cervical mail. These guidelines do not apply to people who have been diagnosed with cervical cancer or pre-cancer of the cervix. These women should have follow-up testing and cervical cancer screening as recommended by their doctor
Cervical cancer testing (screening) should begin at age 25. Those aged 25 to 65 years should have an HPV screening test (primary HPV test) every 5 years. If an HPV screening test (primary HPV test is not available) can be done with an HPV test combined with a Pap 5 test once a year or a Pap test only every 3 years.

The most important thing to remember is regular check-ups, no matter what tests you get.
People over 65 years of age who have had routine screening in the past 10 years with normal results and no history of a diagnosis of CIN2 or higher lesions within the past 25 years should discontinue cervical cancer screening. Once stopped, do not start again. People who have had a total hysterectomy (removal of the uterus and cervix) should stop screening (Pap and HPV tests), unless a hysterectomy is done as a treatment for cervical cancer. Bowel or severe pre-cancer. People who have had a hysterectomy without removal of the cervix (called a partial hysterectomy) should continue to be screened for cervical cancer according to the guidelines above. People who have been vaccinated against HPV should still follow these guidelines for their age groups. Considerations for other patient populations
If a person has a history of high-grade cervical cancer, you should continue testing for at least 25 years after the condition is discovered, even if over 65 years old.
People who are at high risk for cervical cancer because of a suppressed immune system (eg, HIV infection, organ transplantation, or long-term steroid use) or because they were exposed to DES during pregnancy Supply may need to be checked more often. They should follow the doctor's recommendations.
As recommended by relevant organizations and agencies in the United States, including the U.S. Preventive Services Task Force (USPSTF), American Cancer Society (ACS), American Society for Colposcopy and Cervical Pathology (ASCCP); The American Society for Clinical Pathology (ASCP) unanimously made the 2012 recommendations for cervical cancer screening as follows:
Cervical cancer screening should be started at age 21. Women under the age of 21 do not need to be screened. Women ages 21 to 29 should have a Pap test every 3 years. People in this age group don't need an HPV test unless they have an abnormal Pap test result. Women ages 30 to 65 should have a Pap test along with an HPV test (called a "dual test") every 5 years. Or do a separate Pap test every 3 years. Women over 65 years of age who have had routine cervical cancer screening tests for 10 years with normal results do not need to continue to have cervical cancer screening tests. Women over age 65 with a history of CIN2, CIN3, or Carcinoma in situ should continue regular screening for at least 20 years after diagnosis Women who have had their uterus and cervix removed (removal of the uterus) total hysterectomy) for reasons unrelated to cervical cancer and no history of cervical cancer or serious precancerous conditions do not require testing. All women who have been vaccinated against HPV should still have screening tests as recommended for their age group.

2. Importance of cervical cancer screening
In recent years, the primary HPV test has been approved as another cervical cancer screening test. The HPV test looks for infection with high-risk types of HPV that are more likely to cause pre-cancers and cervical cancer. The HPV test can be used alone (primary HPV test) or at the same time as a Pap test (called a co-test).
Screening tests offer the best chance of finding cervical cancer early when treatment can be most successful. Screening can also really prevent most cervical cancers by finding abnormal changes in cervical cells (precancerous) so they can be treated before they have a chance. turn into cervical cancer.
Most cervical cancers are found in women who have never had a Pap test or have not had a recent test. Women with no health insurance and low income levels are less likely to be screened for cervical cancer.
3. Cervical cancer screening tests
The best way to detect cervical cancer early is to have regular screening tests. Tests to screen for cervical cancer are the HPV test and the Pap test. These tests can be done alone or at the same time (called co-tests). Regular screening has been shown to prevent cervical cancer and save lives. The most important thing is to have regular checkups, no matter what tests you get.
Early detection greatly improves the chances of successful treatment and can prevent any early cervical cell changes from becoming cancerous. Being alert to any signs and symptoms of cervical cancer can also help avoid unnecessary delays in diagnosis.
HPV testing
Doctors can now test for HPV (high-risk or cancer-causing types) that are most likely to cause cervical cancer by looking for fragments of their DNA in cervical cells . The test may be done alone or at the same time as the Pap test.
Pap test (Papanicolaou)
A Pap test is a method used to collect cells from the cervix so that they can be analyzed in a laboratory for cancer and pre-cancer.
When cervical screening test results are abnormal
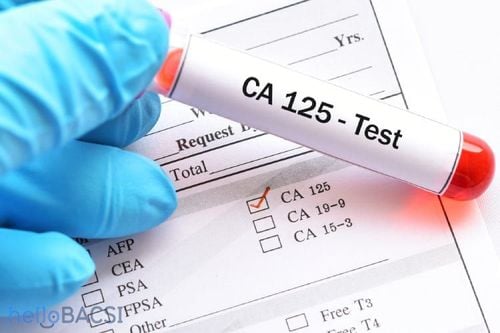
The first step in detecting cervical cancer is usually an abnormal HPV or Pap test result. These results will lead to further tests, which can diagnose cervical cancer.
4. Signs and symptoms of cervical cancer
Women with early and precancerous cervical cancer often have no symptoms. Symptoms usually do not begin until the cancer has become larger and has grown into nearby tissue. When this happens, the most common symptoms are:
Abnormal vaginal bleeding, such as bleeding after vaginal sex, bleeding after menopause, spotting and spotting between periods or periods that are longer or heavier than usual. Bleeding after douching can also occur. Abnormal vaginal discharge - discharge that may contain some blood and may occur between menstrual cycles or after menopause. Pain during sex Pain in the pelvic area Signs and symptoms in more advanced stages may include:
Swollen feet Problems urinating or having a bowel movement Blood in the urine Signs and symptoms This condition can also be caused by conditions other than cervical cancer. However, if you have any of these symptoms, see your doctor right away. Ignoring symptoms can allow the cancer to progress to a more advanced stage and reduce the chances of successful treatment.
For the best chance of successful treatment, don't wait for symptoms to appear. Get regular cervical cancer screening tests.
5. Cervical Cancer Test
The detection of cervical cancer usually begins with an abnormal HPV test or Pap test. This result will lead to further tests that can diagnose cervical cancer or pre-cancer. Pap tests and HPV tests are screening tests, not diagnostic tests. They can't know for sure if you have cervical cancer. An abnormal Pap test or positive HPV test result means that further testing is needed to see if it is cancerous or precancerous.

Find out abnormal cervical screening test results
Current screening test results, along with a person's past test results, determine one's risk of developing cervical cancer . Your doctor will use them to find the next test or treatment. It could be a one-year follow-up screening test, colposcopy, or one of the other procedures discussed below to treat any precancerous stages that may be found.
Since there are many different monitoring or treatment options depending on your risk of developing a particular cervical cancer, it is best to see your doctor for treatment advice
5.1 Testing for people with symptoms cervical cancer or abnormal cervical screening test results Medical history and physical exam
First, your doctor will ask you about your personal and family medical history. This includes information regarding the risk factors and symptoms of cervical cancer. A general physical exam will help assess your general health. You will have a pelvic exam and possibly a Pap test if not already done. In addition, doctors will check the lymph nodes to see if the cancer has spread (metastasized).
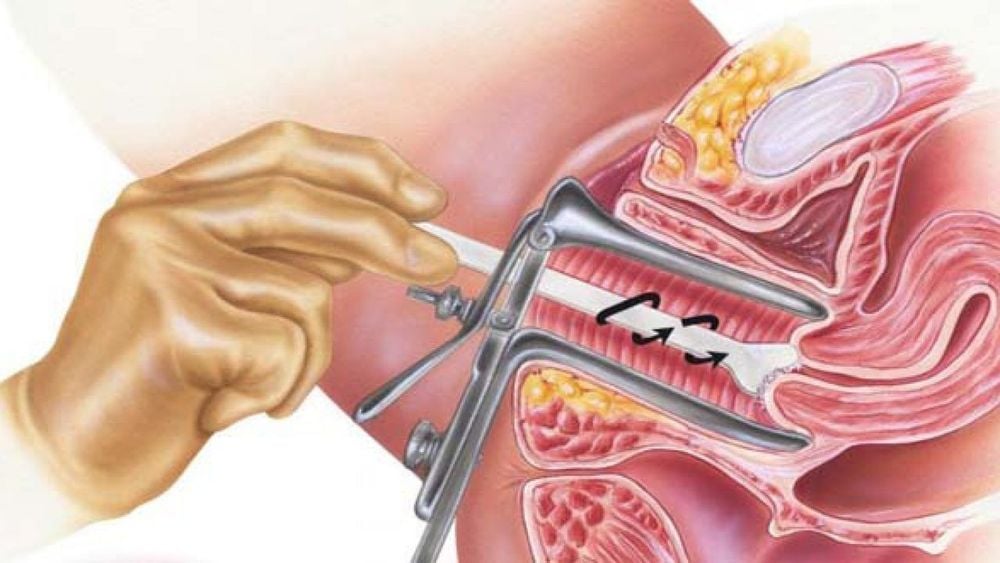
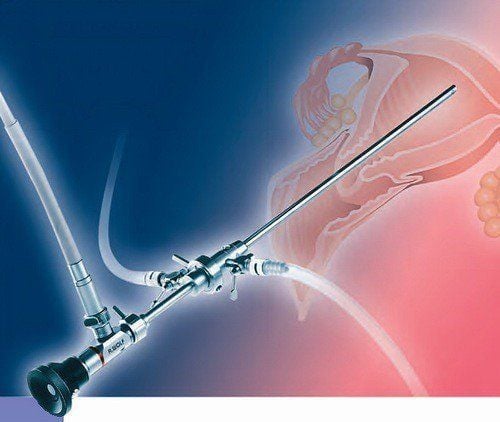
Colposcopy
If you have some symptoms that could be cancer, if your Pap test results show abnormal cells, or if your HPV test is positive, you will most likely need to have a procedure called colposcopy. You will lie on the examination table as you would during a gynecological exam. The doctor will place a speculum into the vagina to help keep it open while examining the cervix with a colposcope. The colposcope is an instrument that is located outside the body and has a magnifying lens. It allows the doctor to clearly see the surface of the cervix up close. Colposcopy itself is usually no more uncomfortable than any other method of spectroscopy. It can be taken safely even if you are pregnant. Like the Pap test, it shouldn't be done during your period.
The doctor will put a weak solution of acetic acid (similar to vinegar) into the cervix to make it easier for you to see any abnormal areas. If an abnormal area is seen, a small piece of tissue is removed (biopsy) and sent to a laboratory for careful analysis. A biopsy is the best way to know for sure if an abnormal area is precancerous, or actually cancerous.
Types of cervical biopsies
Several types of biopsies can be used to diagnose cervical precancer and cancer. If a biopsy is able to completely remove all abnormal tissue, it may be the only treatment needed.
Colposcopy biopsy
For this type of biopsy, the cervix is first examined with a colposcope to look for abnormal areas. Use tissue biopsy forceps to apply to the abnormal area on the surface of the cervix. The biopsy procedure may cause mild pain, brief pain, and light bleeding afterward.
Colposcopy
If colposcopy does not show any abnormal areas or changes are not seen (area at risk of HPV infection and pre-cancer) by colposcope, then cervical curettage must be used uterus for examination.
A narrow instrument ( scraper or brush ) is inserted into the cervical canal. A scraper or brush is used to scrape the inside of the cervical canal to remove some pieces of tissue, which are then sent to a laboratory for examination. After this procedure, the patient may feel some cramping and may also experience light bleeding.

Cervical cone
The doctor will remove a cone-shaped piece of tissue from the cervix. The base of the cone is formed by the external neck (outer part of the cervix), and the point or apex of the cone is from the endometrial duct. The tissue removed in the cone includes the transformation zone (the transition zone between the lateral and medial necks, where cervical precancers and cancers are most likely to begin). Cone biopsy can also be used as a treatment to completely remove many precancerous and some very early cancers.
Commonly used methods for cone biopsies are loop electrosurgical excision (LEEP), also known as large loop excision of the variable area (LLETZ), and cold knife cone biopsy .
LEEP or LLETZ procedure: In this procedure, tissue is removed with a thin wire loop that is heated electrically and acts like a small knife. For this procedure, a local anesthetic is used and can be done in the doctor's office. Cold knife cone biopsy: This is done in a hospital. A surgical knife or a laser is used to remove tissue instead of a heating wire. You will be given anesthesia during the procedure (general anesthesia, either spinal or epidural,). Complications that can occur with conical resection include bleeding, infection, and narrowing of the cervix.
Women who have had any type of cerclage can still get pregnant, but if a large amount of tissue has been removed, the woman may be at higher risk of preterm birth.
5.2 For people with cervical cancer If the biopsy shows cancer, the doctor may order some tests to check if the cancer has spread. Many of the tests described below are not applicable to all patients. Decisions about which of the following tests to use are based on the results of a physical exam and biopsy.
Cystoscopy, hysteroscopy, proctoscopy:
These are often done in women with large tumors. They are not needed if the cancer is found early.
During cystoscopy, a thin tube with a lens and light is placed into the bladder through the urethra. This allows your doctor to examine your bladder and urethra to see if cancer has grown into these areas. Biopsy samples may be removed during cystoscopy for laboratory examination. Cystoscopy can be performed under local anesthesia, but some patients may need general anesthesia. Your doctor will tell you what to expect before and after the procedure.
Colonoscopy is an examination of the rectum through a lighted tube to look for the spread of cervical cancer into your rectum.
Your doctor may also do a pelvic exam while you are under anesthesia to see if the cancer has spread beyond the cervix.
Chest X-ray:
Your chest may be X-rayed to see if cancer has spread to your lungs.
Computed tomography (CT):
CT scan is usually done if the tumor is larger or if there is concern about the spread of the cancer.
Magnetic resonance imaging (MRI)
An MRI scan to examine soft tissue parts of the body is sometimes better than other imaging tests, like a CT scan. Your doctor will decide which imaging test is best to use in your situation.
PET scan
For a PET scan, a mild form of radioactive sugar (called FDG) is injected into the bloodstream and mainly collects in cancer cells.
PET/CT scan: Often a PET scan is combined with a CT scan using a special machine that can do both at the same time. This allows the doctor to compare areas of higher radioactivity on a PET scan with a more detailed image on a CT scan. This is the most commonly used type of PET scan in patients with cervical cancer.
This test can help see if cancer has spread to the lymph nodes. A PET scan can also be helpful if your doctor thinks the cancer has spread but doesn't know where.
Intravenous pyelogram (IPV)
An intravenous pyelogram (IVP) is an X-ray of the urinary system that is done after a special dye is injected into a vein. This test can find abnormal areas in the urinary tract caused by the spread of cervical cancer. The most common finding is that the cancer has blocked the ureter (the tube connecting the kidney to the bladder). IVP is rarely used for cervical cancer patients because CT and MRI are also very good at finding abnormal areas in the urinary tract, as well as other areas not seen with IVP.
In order to improve the quality of diagnosis and treatment, Vinmec International General Hospital has applied the ThinPrep Pap Test for early detection of cervical cancer, this new method is now commonly used in the US, Europe. ThinPrep Pap Test has made a breakthrough compared to the traditional Pap smear method, through membrane controlled cell transfer technology, which increases the sensitivity and specificity in detecting precancerous cells. , especially adenocarcinoma cells, a type of cancer cell that is difficult to detect.
At Vinmec, the application of modern methods and procedures to ensure sterility helps to achieve the most accurate results. Screening results are returned to your home with specific advice and recommendations for the patient
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.