This is an automatically translated article.
Article written by Dr. Pham Anh Tuan - Vinmec Institute of Stem Cell and Gene Technology
The blood-brain barrier (BBB) is a layer of cells that covers the blood vessels in the brain and regulates the entry of molecules from the blood into the brain. Increased "permeability" or degree of leakage across the blood-brain barrier of molecules, observed in some cognitive disorders and harmful effects on the nervous system; therefore, understanding the regulation of blood-brain barrier permeability is crucial for the development of better therapies for such disorders.
In a study recently published in Nature Communications, a research team led by Professor Hiroaki Wake of Nagoya University School of Medicine showed that microglia - the brain's resident immune cells - protect the The blood-brain barrier from being damaged by "systemic inflammation," a chronic inflammatory condition linked to factors such as smoking, aging, and diabetes, and leading to an increased risk of neurodegenerative disorders. However, these microglia can change their behavior and increase blood-brain barrier permeability, thereby damaging it.
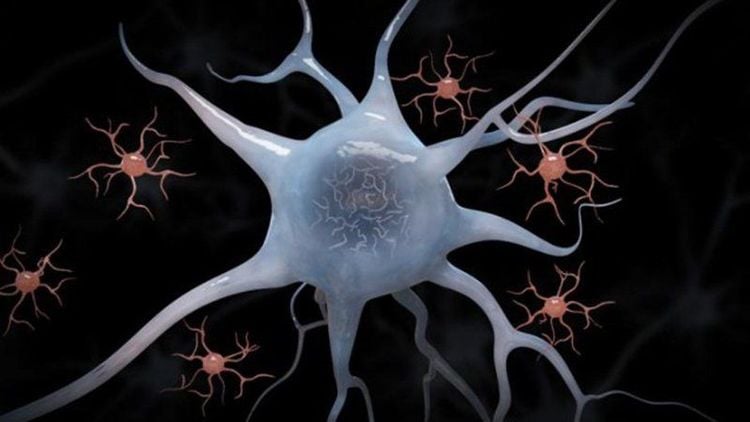
Microglia - tế bào miễn dịch thường trú của não
Professor Wake commented "We have known for a long time that microglia can be activated by inflammation, so we were interested in the question of whether microglia could regulate blood-brain barrier permeability." To explore this, the team worked with mice that were genetically engineered to produce fluorescent proteins in microglia. This fluorescent labeling allows researchers to use a two-photon excitation microscope, a fluorescence imaging technique that allows imaging of living tissue up to about a millimeter thick, to study the interactions of microglia and the blood-brain barrier in live rats. The investigators also injected the mice with fluorescent molecules that can cross the blood-brain barrier only when the barrier is damaged becomes permeable. Based on observing the positions of these fluorescent molecules, the team was able to study how microglia interact with the blood-brain barrier and blood-brain barrier permeability under different conditions.
A key point of interest is the inflammation induced by injecting mice with an inflammatory agent, which leads to migration of microglia to blood vessels and increases the permeability of the blood-brain barrier within days. Then, initially, microglia acted to protect the blood-brain barrier and limit increased permeability, but as inflammation progressed, microglia reversed their behavior by attacking components of the barrier. blood-brain, thereby increasing the permeability of the barrier. Leakage of molecules into the brain has the potential to cause widespread inflammation and thus damage to nerve cells.

Sự rò rỉ microglia vào trong não là nguyên nhân gây tổn thương các tế bào thần kinh
These results clearly suggest that microglia play a dual role in regulating blood-brain barrier permeability. Professor Wake commented that they aim to identify therapeutic targets on microglia to regulate blood-brain barrier permeability, because drugs designed for such targets can be used to modulate blood-brain barrier permeability. Treats neurological and psychiatric diseases by limiting inflammatory responses in the brain.
As the scientists noted in their study, uncontrolled inflammatory responses in the brain can cause a range of cognitive disturbances and adverse neurological effects, and drugs that target microglia can help patients avoid such problems by maintaining the integrity of the blood-brain barrier. However, the results of the study offer hope for the development of therapies that can "force" microglia to promote integrity and prevent microglia from switching to behaviors that destroy the blood-brain barrier.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.