This is an automatically translated article.
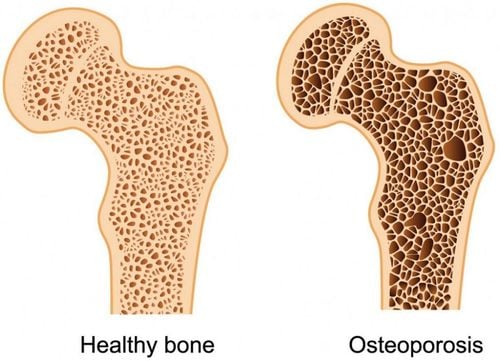
Osteoporosis is a disease characterized by low bone mass and impaired bone structure, which can lead to an increased likelihood of fractures. Common risk factors for osteoporosis are smoking, alcoholism, and physical inactivity. However, there is also an underappreciated potential cause due to the use of drugs that affect bone density.
1. Corticosteroids
The most common secondary cause of osteoporosis and the third most common cause overall is systemic corticosteroid use. Glucocorticoids are widely used and effective in the treatment of many diseases such as lung disease, rheumatism, digestive, dermatological and especially autoimmune disorders. The risk of bone loss is highest within the first 6 to 12 months of long-term therapy and is dose dependent. Many studies have evaluated comorbidities associated with steroid-induced osteoporosis; An estimated 30% to 50% of patients receiving long-term systemic steroids will eventually experience a fracture.
There are many factors that contribute to corticosteroid-induced bone density loss. Glucocorticoids decrease bone formation by increasing osteoclast apoptosis and decreasing growth factors involved in bone remodeling. On the other hand, steroids have also been shown to induce calcium deficiency by decreasing gastrointestinal calcium absorption from the gut and increasing renal excretion of calcium. All of these factors play a role in the pathophysiology of steroid-induced osteoporosis.
Therefore, risk awareness and prevention of bone loss are important aspects of any steroid regimen. Where possible, alternatives to long-term corticosteroid therapy should be used to avoid not only osteoporosis but also the many other side effects of corticosteroids. However, this is not always possible and the positive effects of corticosteroids in certain settings may outweigh the effectiveness of other therapies. Nevertheless, short-term steroid measures should be taken where possible and dose reduction or other dosage forms, such as inhaled or topical regimens, should be taken to prevent systemic complications.
The prevention of bone loss, which is important in patients requiring systemic steroids, can be improved by supplementation with calcium (1,200 to 1,500 mg/day) and vitamin D (400 to 800 units/day) . Concurrently, patients requiring chronic steroid therapy should also receive bisphosphonates, alendronate, or risedronate, for the prevention and treatment of corticosteroid-induced osteoporosis. Bisphosphonates act through inhibition of osteoclast activity and reduction of bone resorption.
Có nhiều yếu tố gây suy giảm mật độ xương do corticosteroid
2. Antiepileptic drugs
Some anticonvulsants or antiepileptic drugs can cause bone loss.
Examples of antiepileptic drugs include phenytoin, phenobarbital, carbamazepine and primidone. These drugs are strong inducers of the CYP-450 isoenzyme, and the rate of bone loss in those given this class of drugs is nearly double that of the general population. The mechanism is that these drugs both induce the hepatic enzyme CYP-450, leading to rapid metabolism of vitamin D and possibly estrogen. At the same time, the drug is also associated with decreased calcium absorption causing secondary hyperparathyroidism and increased bone turnover. At therapeutic levels, phenytoin and carbamazepine act directly on bone by inhibiting osteoblast cells. On the other hand, phenytoin also inhibits the secretion of osteocalcin - a hormone that regulates calcium in the bones.
To counteract the loss of bone density caused by traditional antiepileptic drugs, a newer generation of drugs with a lower rate of liver induction should be used. While long-term studies are still needed to assess whether the new class of drugs causes bone loss, the results so far look promising. In addition, vitamin D and calcium supplementation is necessary to prevent bone loss in patients who are stable on older medications. Prophylactic doses of at least 400 international units (IU) of vitamin D and 1,000 to 1,500 mg of calcium are recommended for people at high risk of osteoporosis.
3. Heparin
Unfractionated heparin is also associated with drug-induced osteoporosis. This complication is often seen when long-term and high-dose treatment is required. However, as the use of new generation low-molecular-weight heparins has become more common and readily available in the outpatient setting, the risk of bone loss has also been reduced.
The exact cellular mechanism by which heparin causes bone loss is not completely understood. It is hypothesized that heparin accelerates bone resorption by stimulating osteoclasts and inhibiting osteoclast function, leading to decreased bone density. At this time, the activity of PTH is also stronger, increasing the release of calcium and phosphorus from the bones into the blood to raise the serum concentration; PTH is usually released in response to low serum calcium levels.

Heparin không phân đoạn cũng có liên quan đến chứng loãng xương do thuốc
4. Progestin
One of the drugs that has recently been linked to osteoporosis is a progestin. Progestin is a hormone commonly used in many forms of contraception, as well as in hormone replacement products, and is therefore used in women of all ages. The progestin product commonly associated with bone loss is medroxyprogesterone acetate, an injectable form of birth control.
Since the risk of bone loss is observed to increase after two years of continuous progestin use, since its widespread use, the prevention of osteoporosis should also be considered through the promotion of supplementation. calcium and limited use time. At this point, other forms of birth control can be substituted, such as the combined pill, if longer-term contraception is needed.
The mechanism of medroxyprogesterone for bone loss is dose-dependent and the patient's estrogen levels due to ovarian suppression of estrogen production. Estrogen has a protective effect against bone loss, and low levels of estrogen can lead to a decline in bone mass. At the same time, medroxyprogesterone also inhibits gonadotropin secretion of LH, FSH and also exhibits corticosteroid-like properties, so it can reduce osteoblast differentiation, affecting bone density.
5. Other drugs
The drugs listed above have the most common risk of osteoporosis. However, other drugs have also been linked to bone loss less commonly, namely:
Methotrexate may increase the risk of osteoporosis when used in very high doses, such as in cancer patients letters. The mechanism is not fully understood but is thought to involve an imbalance of bone resorption and formation.
Loop diuretics (eg, furosemide) may also decrease bone mass by increasing renal excretion of calcium.
Another potential cause of bone loss is excess thyroid hormone. This usually occurs only when thyroid-stimulating hormone levels are virtually undetectable due to oversupply, causing bone demineralization.
Aluminum-containing antacids can bind calcium in the gastrointestinal tract and lead to decreased calcium absorption.
Lithium has been shown to increase PTH secretion, which can cause calcium release from bone to increase serum calcium levels.
Several animal models have shown increased turnover and bone loss with the use of cyclosporin and tacrolimus.
Prolonged use of warfarin has been associated with increased fracture events.
In a nutshell, drug-induced osteoporosis is a preventable condition. Accordingly, identify potential risks when taking drugs that affect bone density, monitor and use preventive measures, such as promoting a diet rich in calcium and vitamin D, quitting smoking, avoiding Drinking too much alcohol or caffeine can significantly improve a patient's quality of life.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: uspharmacist.com, webmd.com