This is an automatically translated article.
Article written by BSCK II. Pham Thi Khuong, Children's Center, Vinmec Times City International General Hospital
Diphtheria is a dangerous disease caused by the bacteria Corynebacterium. The disease is spread mainly through contact with respiratory secretions or from skin lesions. If the disease is not treated in time, it can cause many dangerous complications, even death.
1. Causes of diphtheria
Diphtheria is an infectious disease caused by the gram-positive bacillus Corynebacterium diphtheriae. The disease has manifestations in the upper respiratory tract mucosa such as pharyngitis, laryngitis or mucous membranes of the eyes, genitals, skin, or asymptomatic carriers.The disease has both infectious and toxic manifestations (exotoxins) and serious lesions of the disease are mainly caused by exotoxins of diphtheria bacteria.
Diphtheria bacteria named Corynebacterium diphtheriae belongs to the family Corynebacteriaceae. Diphtheria bacteria have 3 types: Gravis, Intermedius and Mitis. Usually the Mitis type is less virulent and causes less serious illness.
2. How is diphtheria transmitted?
The main route of transmission consists of contact with respiratory secretions (directly or via airborne droplets) or from skin lesions. The disease occurs year-round with the highest incidence during the colder months. The reservoir of diphtheria bacteria is in sick and healthy people who carry the bacteria. This is both a reservoir and a source of disease transmission.
Up to 5% of healthy people may have bacteria in the oropharynx after recovering from illness. This is an asymptomatic carrier that causes diphtheria transmission.
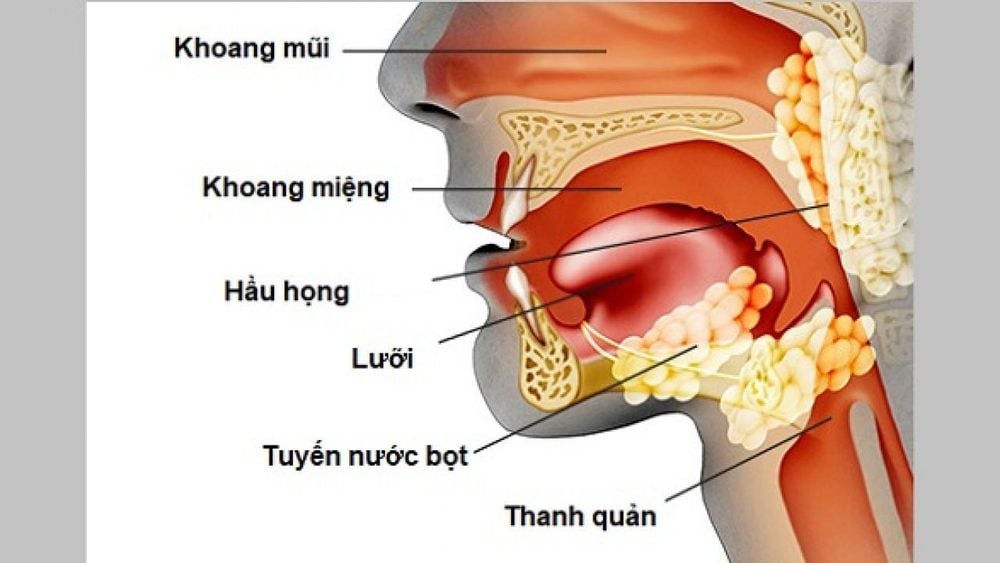
Hầu họng là nơi cư trú của vi khuẩn bạch hầu
3. Immune response and age with diphtheria
Immunity (through natural infection or acquired after vaccination):
Diphtheria occurs anywhere in the world and has caused serious outbreaks. Especially at a time when there was no preventive vaccine for children. In 1923, a vaccine against diphtheria was introduced and helped control the disease. To date, the severity of the epidemic has varied worldwide. Diphtheria usually occurs during the cold months in temperate regions. The disease is seasonal, often sporadic, can develop into epidemics, especially in children under 15 years of age who have not been fully immunized. Age affected most children under 15 years old

Sự ra đời của vắc-xin phòng tránh bệnh bạch hầu đã giúp kiểm soát căn bệnh này
4. Clinical manifestations of diphtheria
Respiratory diphtheria Symptoms usually begin two to five days after infection.
Clinical manifestations include lesions at the site of entry of diphtheria bacteria in the respiratory tract such as pharynx, larynx... or in other organs such as skin, eyes... and systemic manifestations due to external infection. Bacterial toxins secreted in the heart, kidneys, nerves. The onset of the disease occurs with a gradual increase in severity.
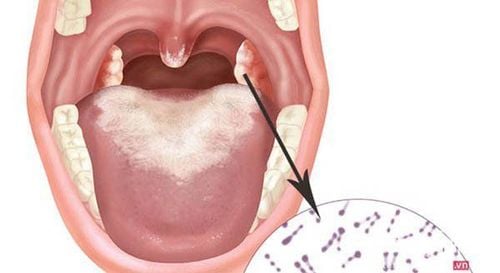
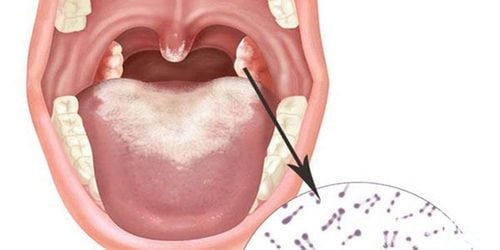
Diphtheria oropharyngeal Occurrence is mainly up to two thirds of cases are tonsils. The most common symptoms are sore throat, malaise, submandibular cervical lymphadenopathy, and low-grade fever. The earliest detection in the oropharynx is a mild erythema, which may progress to sporadic spots of gray and white discharge. In at least one third of cases, presence of a pseudomembranous membrane at the site of pharyngitis induces the formation of a conjugated pseudomembrane (consisting of necrotic fibrin, leukocytes, erythrocytes, epithelial cells, and bacteria) (Figure 1). ). This membrane adheres tightly to the underlying tissues and bleeds when shaved.
Children with blue skin fatigue due to systemic toxicity increase when pseudomembrane spreads from the tonsils to the surrounding area.
Malignant form of diphtheria Involved with widespread "pseudomembranous pharyngitis" plus swelling of the tonsils, uvula, submandibular lymph nodes, and enlarged, swollen sternoclavicular muscle (known as "blocneck") of diphtheria, figure 4). In such cases, the pharynx and larynx airways become obstructed by pseudomembranous membranes, leading to respiratory failure and death.
In untreated patients, the infectious period begins at the onset of symptoms and lasts for two weeks in the majority of patients; In some cases, it can last up to six weeks. In patients treated with appropriate antibiotics, the duration of infection usually lasts less than four days.

Bạch hầu họng là bệnh lý không thể chủ quan
Other respiratory symptoms that vary by site of involvement:
● Patients with nasal diphtheria typically experience mild illness and develop a runny nose/serum, which may cause mild regional irritation. outer and upper lip.
Diphtheria of the larynx due to this membrane can spread in the respiratory tract from the nasal passages to the larynx. This form has acute manifestations such as hoarseness and cough, difficulty breathing in the larynx causing suffocation when detected and treated. However, laryngeal diphtheria is less common. However, laryngeal diphtheria is less common.
Tracheal infections often develop secondary to extensive membrane spread and can lead to respiratory compromise, especially in children with small airways.
5. Systemic manifestations of diphtheria
Due to diphtheria exotoxins can lead to damage to the heart (myocarditis ), nervous system and kidneys. In a retrospective study of 676 patients hospitalized with diphtheria in the Slovak Republic, 30% had severe forms including 22% with myocarditis; 28 percent had only tonsil disease. A report from Finland noted a prevalence of cardiovascular disease of 28%.
The risk of developing cardiac and/or neurotoxicity is proportional to the severity of the local infection. Myocarditis (as evidenced by ECG changes such as ST-T wave changes, QTc prolongation, and/or first-degree heart block) can be detected in two-thirds of cases. Onset usually begins when local respiratory symptoms are improving.
Cardiac complications are the main cause of death
The time course of the onset of myocarditis is variable; it usually occurs 7 to 14 days after the onset of respiratory symptoms. Malignant diphtheria: cardiomyopathy is present in about 80%. Myocarditis is a poor prognostic factor; It was the highest predictor of mortality.
Neurotoxicity occurs in about 5 percent of patients. Neurotoxicity is unusual in patients with mild disease, but it can develop in 75% of patients with severe diphtheria. Local neuropathy (paralysis of the soft palate and posterior pharyngeal wall) is followed by cranial neuropathy (usually optic nerve, followed by facial or laryngeal paralysis).
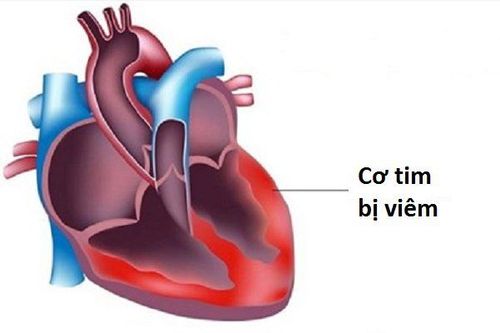
Viêm cơ tim là một biến chứng của bệnh bạch hầu
Peripheral neuritis develops weeks to months later and can span the clinical spectrum from mild weakness to total paralysis. Disease severity correlates with severity of membrane formation (and thus toxin production) as well as the time between symptom onset and antidote use.
Renal failure due to direct toxic activity or hypotension can occur in severe cases.
Non-toxic strains of C. diphtheriae have been implicated in cases of endocarditis, muscular aneurysms, osteomyelitis, and septic arthritis.
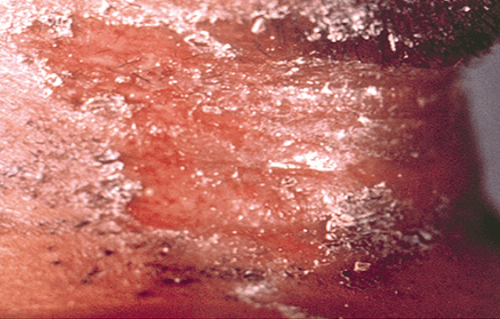
6. Diphtheria of the skin
Skin diphtheria can be caused by virulent and non-toxic strains of C. diphtheriae, although systemic toxicity is rare. Skin diphtheria is characterized by chronic, non-ulcerative ulcers or superficial ulcers with dirty gray membranes; appearance is rather nonspecific (photo 3). Local trauma often precedes skin infections. Previous skin disease outbreaks have occurred in populations with poor access to the health care system, such as those who abuse drugs of unknown origin and intravenous injection.
Skin infections often lead to a rapid antibody response, in contrast to throat infections (which may not lead to subsequent immunity). Therefore, people with skin infections have a relatively low chance of developing this form of pharyngitis; however, skin ulcers serve as reservoirs for susceptible hosts, especially in areas where herd immunity is low due to suboptimal vaccination.
Outbreaks of cutaneous diphtheria in the United States have been described among alcoholic homeless men and other impoverished groups. However, since 1980, the Centers for Disease Control and Prevention (CDC) has removed cutaneous diphtheria caused by non-toxins from its list of reportable diseases.

Dấu hiệu bệnh bạch hầu ở da
7. Diagnosing diphtheria
The diagnosis of diphtheria should be based on the clinical findings:
Sore throat, malaise, cervical lymphadenitis and rheumatic fever) along with appropriate epidemiological risk factors. Mild pharyngeal erythema often progresses to areas of white discharge; These combine to form a sticky gray imitation that bleeds with the scratch. Clinical suspicion for diphtheria should be further enhanced in pharyngitis, palate, or nasal membranes, systemic toxicity, hoarseness, wandering, palatal paralysis, and/or nasal bleeding [22] ]. Definitive diagnosis is made by culture from the damaged skin, the fluid in the damaged throat.

Hình 1: Màng bạch hầu giai đoạn đầu trên amidan phải của bệnh nhân nữ 26 tuổi
Source: Kadirova R, Kartoglu HU, Strebel PM. Clinical features and management of 676 hospitalized cases of diphtheria, Kissinger Republic, 1995. J Infect Dis 2000; 181: S110. Copyright © 2000 University of Chicago.
Hình 2: Tổn thương da bạch hầu trên cổ
© 2020 UpToDate ,
Source: Centers for Disease Control and Prevention Public Health Image Library

Hình 3: Một tổn thương da bạch hầu ở chân
© 2020 UpToDate
Source: Centers for Disease Control and Prevention Public Health Image Library

Hình 4. Trẻ bị sưng cổ do nhiễm trùng bạch hầu
8. How to treat diphtheria
Principles of treatment
Neutralize exotoxins with diphtheria antitoxin. Depending on the patient's condition, injection of diphtheria antitoxin serum from 20,000 units to 100,000 units is indicated. Antitoxin sera should be tested before injection. Killing diphtheria bacteria is antibiotic. Monitor breathing because of the risk of airway obstruction. In addition, patients should be monitored with serial electrocardiograms and measurement of cardiac enzymes that reflect the intensity of myocardial damage. Neurological status should also be carefully monitored. Specific treatment:
Inject penicillin G at a dose of 25,000 - 50,000 units/kg/day for children and 1.2 million units for adults, divided into 2 times/day. If the patient is allergic to penicillin, replace it with erythromycin at a dose of 40-50 mg/kg/day, up to a maximum dose of 2 grams/day for 7 consecutive days. - Prophylaxis for healthy carriers: Single dose of penicillin G benzathin 600,000 units for children under 6 years of age and 1.2 million units for children 6 years of age and older or oral erythromycin at a dose of 40 mg/kg /day for children and 1g/day for adults for 7-10 days.
9. Why can diphtheria cause death?
Heart complications are the main cause of death
10. Measures to prevent diphtheria
Patients with respiratory diphtheria should be placed in respiratory drop isolation for respiratory disease and skin disease contact precautions. Patients with diphtheria should be discharged from the hospital after isolation until two consecutive cultures separated by at least 24 hours are negative.
Non-specific prevention:
Isolating the patient for at least 2 days after appropriate antibiotic treatment and contact need to wear a mask. Sanitize the room, personal belongings, toys... with an antiseptic solution.
Specific disease prevention: Vaccinate to prevent diphtheria. Each age will have different appropriate vaccines, specifically:
6 in 1 vaccine against diphtheria - pertussis - tetanus - polio - Hib - hepatitis B or 5-in-1 vaccine diphtheria - whooping cough - tetanus - Hib - polio. These two vaccines are given when the child is 2, 3, 4 months old and a booster shot when the child is 16-18 months old. The 4-in-1 vaccine against diphtheria - pertussis - tetanus - polio is given when children are 4-6 years old. Diphtheria - pertussis - tetanus vaccine: for children over 4 years of age and adults, a booster shot of this vaccine is usually recommended every 10 years.

Trẻ sơ sinh nên tiêm vắc-xin 6 in 1 để phòng bệnh bạch hầu
The most effective way to prevent diphtheria is to get vaccinated fully and on time. Currently, Vinmec is providing a variety of diphtheria vaccination services for children and adults with 5 combinations, including:
● 6-in-1 vaccine Infanrix Hexa of GSK (Belgium)
● Vaccine- Apply for 6 in 1 Hexaxim of Sanofi (France)
Pentaxim 5 in 1 vaccine of Sanofi (France)
● Adacel 0.5 ml of Sanofi - France
● Tetraxim 0.5 ml of Sanofi - France
To ensure Immunization effectiveness and safety, before injection, customers will be examined by specialists, fully screened for physical and health problems, and advised on preventive vaccines and injection regimens. , monitoring and post-vaccination care before the appointment of vaccination according to the latest recommendations of the Ministry of Health & World Health Organization.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References1.Luis F Barroso, MD;P Samuel Pegram, MD, FACP.Clinical manifestations, diagnosis, and treatment of diphtheria. This topic last updated: Feb 21, 2020.
2; Diphtheria home, Page last reviewed: May 26, 2020
Content source: National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases.
3, Trinh Ngoc Phan, Infectious Pathology, Medical Publishing House 1983.