This is an automatically translated article.
Posted by Master, Doctor Luu Thi Bich Ngoc - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International HospitalIschemic colitis is an inflammatory condition of the colon caused by insufficient blood supply, causing a lack of oxygen in the tissues. The severity and consequences of the disease vary widely, depending on the underlying condition. Medical imaging techniques help to make early diagnosis of ischemic colitis and guide timely intervention.
1. What is ischemic colitis?
Ischemic colitis includes several clinical entities, all of which ultimately result in inadequate blood supply to a segment or the entire colon. This disease leads to ischemic necrosis of varying degrees of severity, which can range from localized mucosal surfaces to complete transmural necrosis of the colonic wall.
Intestinal ischemia is mainly a disease of old age due to atheroma of the mesentery. Other causes include occlusive disease, vasculitis, fibromuscular hyperplasia, aortic aneurysm, abdominal trauma, disseminated intravascular coagulation, irradiation, and hypovolemic or endotoxin shock. In the case of mesenteric infarction (embolism or thrombosis), the patient has a 90% mortality risk while the non-embolic disease has a mortality rate of only 10%.
In contrast, venous infarction occurs in younger patients, usually after abdominal surgery. Patients may experience intermittent, intermittent abdominal pain that may be associated with vomiting, diarrhea, or rectal bleeding.
Regardless of the etiology, the diagnosis of ischemic colitis is mainly based on imaging studies instead of relatively vague clinical manifestations. Of these, abdominal X-rays are usually done in most cases involving acute problems in the abdomen. Next, contrast-enhanced computed tomography (CT) is the best test after radiography alone, as it can rule out many other causes of abdominal pain and can also diagnose ischemia. intestinal tract. MRI is mostly useful for magnetic resonance angiography, especially in people with compromised kidney function. Ultrasound is a noninvasive technique that can provide useful information, particularly in the investigation of chronic mesenteric ischemia, but is not conclusive in excluding mesenteric ischemia. . For angiography, this tool has a limited role in cases of colon ischemia.
Details for each specific medical imaging technique are as follows:
1.1 X-ray X-ray features on plain radiographs to diagnose ischemic colitis include:
Dilation part of the colon can be seen early. The presentation may not be the same as that of ulcerative colitis with mucosal edema (thumbprint) and a pseudo-mucous appearance. When both the small and large intestines are affected by ischemic injury, the small intestine may also become dilated with thickening of the intestinal loops.
Over time, the intestinal wall becomes thickened and edematous, containing a large amount of secretions. As the edema worsens, the colon wall loses its folds and becomes smooth. Air bubbles appear in the intestinal wall, which is an evidence of intestinal necrosis.
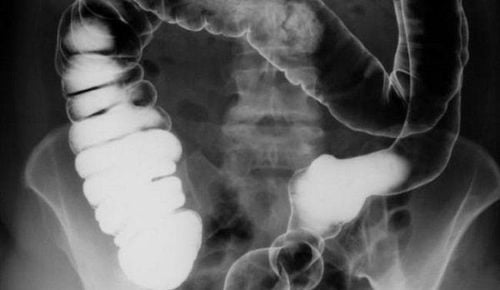
Features of ischemic colitis on radiographs with barium enema. Examination with barium enema in the acute phase showed constriction of the intestinal wall and effacement of mucosal folds. Multiple layers of scaly or fingerprinted mucosa are seen along the border of the intestine. With further progression of mucosal edema, the folds become thicker and indistinct.
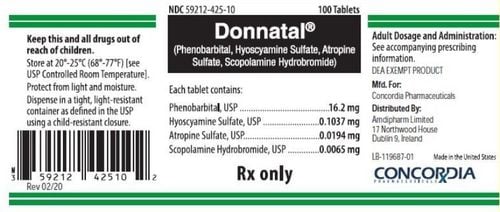
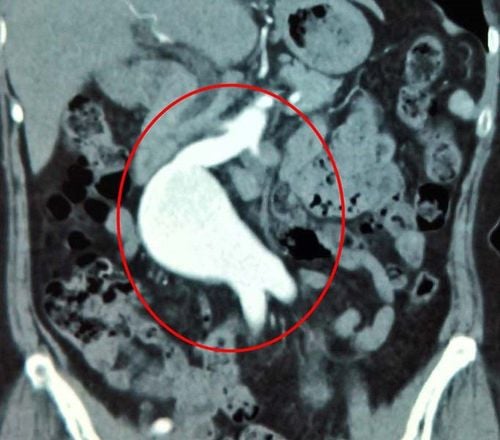
1.2 Computed tomography Computed tomography (CT) with contrast injection has been used as a diagnostic tool in patients with suspected intestinal ischemia. CT not only depicts vascular changes but also reveals changes in the intestinal wall, often in association with other intra-abdominal pathological findings. Contrast-enhanced CT also provides information regarding the hemodynamics of intestinal blood flow.
CT is considered a valuable noninvasive tool in the diagnosis of mesenteric ischemia. The specific CT findings to confirm the diagnosis of intestinal ischemic colitis depend on the degree of ischemia, the length of the bowel loops involved, and whether both the large and small intestine are affected with The features are as follows:
Mesenteric thromboembolism Internal air or portal vein Segmental thickening of intestinal wall No enhancement of intestinal wall. Abnormal narrowing of the lumen due to mucosal edema May be dilated proximal bowel ischemic Nonspecific signs of intestinal ischemia, including bowel obstruction, mesenteric edema, mesenteric vascular adhesions and ascites.
1.3 Magnetic resonance imaging Magnetic resonance imaging (MRI) for the diagnosis of ischemic colitis has a sensitivity comparable to that of CT. Accordingly, MRI may be useful in characterizing intestinal wall changes and demonstrating mesenteric vascular abnormalities. As with CT, the use of additional contrast in MRI will allow assessment of kinetic changes in the intestinal wall.
In addition to the fact that MRI is as sensitive as CT in the diagnosis of intestinal ischemia, this tool also has the added advantage of not using ionizing radiation. At the same time, MRI also has a significant role in the characterization of small thrombus in the small vessels of the mesentery.
1.4 Ultrasound The relatively large amount of air in the intestinal lumen frequently precludes the ability of abdominal ultrasonography to investigate colonic changes, which are most clearly concentrated around the hepatic and splenic flexure.

In the early stages, the ischemic bowel segment may show increased motility, then gradually decrease. The intestinal wall becomes thickened, hemorrhagic, and edematous, giving rise to hypoechoic areas. Furthermore, if air is found in the portal vein, this is a poor prognostic sign.
Color flow Doppler ultrasound is performed after the patient fasts overnight to minimize intestinal gas. At this point, Doppler ultrasound will be effective in assessing the flow of blood vessels. Compared with CT or MRI, ultrasound is a relatively sensitive and noninvasive technique that can provide useful information on mesenteric ischemia. However, this tool is highly subjective, and a dilated colonic framework filled with gas during bowel obstruction or obstruction may preclude adequate visualization of the vascular system on ultrasound.
1.5 Angiography Angiography has been shown to have a limited role in the diagnosis of colonic ischemia. However, for certain indications, angiography can be an invaluable tool.
When ischemia affects only the colon, blood flow on the angiogram may remain normal. However, as soon as vascular occlusion is present, angiography will show a vascular defect.
At the same time, with the increasing inflammatory bowel response, angiography can also show dilated arteries before the obstruction, contrast medium accumulation in the intestinal parenchyma, and thickening, filling of the venous inflow. Soon.
In the case of superior mesenteric or inferior mesenteric vein thrombosis, the veins may not be seen and may depict accessory vein filling. Superior mesenteric or inferior mesenteric artery fistulas are easily identified by angiography. Stealing vascular syndrome is usually diagnosed by inferior mesenteric angiography.
In summary, ischemic colitis is an often overlooked clinical condition while the colon is the most common ischemic region in the gastrointestinal tract. However, when thinking about this diagnosis with its associated suggestive risk factors, an ordered approach with the right imaging tools helps in timely recognition and surgical intervention when indicated. .
Vinmec International General Hospital is one of the leading hospitals in the country in terms of examination, diagnosis and treatment of digestive diseases. Therefore, when there are signs of disease onset or need advice on intensive treatment, patients can go to the hospital for advice and examination by a team of doctors and specialists.
The hospital has a system of modern equipment and machinery to help diagnose diseases accurately. Create peace of mind for customers.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.