This is an automatically translated article.
Primary hepatocellular carcinoma is cancer arising from liver cells, the most common of all liver tumors. Hepatocellular carcinoma is the third leading cause of cancer-related death worldwide.1. Causes of primary hepatocellular carcinoma
Primary hepatocellular cancer is a common disease in our country. Recorded at the Hanoi Oncology Hospital, hepatocellular carcinoma ranks third after stomach and bronchial cancers. Most common in men aged 50-60. The prevalence according to age in men 19.7/100,000 in women 8.3/100,000.
Chronic infection with hepatitis B or C virus is the most common cause of hepatocellular carcinoma. People with either of these viruses have a significantly higher risk of developing liver cancer than otherwise healthy people, because both diseases carry a higher risk of developing cirrhosis.
Other risk factors for hepatocellular cancer include:
Type 2 diabetes: People with diabetes, especially if they have hepatitis or regularly drink a lot of alcohol, are more likely to develop cancer. liver cells. Family history: If your mother, father, brother or sister had hepatocellular carcinoma, they have a higher risk of developing the disease.

Bệnh tiểu đường type 2 nếu bị viêm gan có thể dẫn đến ung thư tế bào gan
Heavy alcohol use: Drinking more than six glasses of alcohol a day for a long time can lead to cirrhosis. This increases the risk of hepatocellular carcinoma. Long-term exposure to aflatoxin : Aflatoxin is commonly found in moldy foods Low immunity: People with weakened immune systems, such as those with HIV/AIDS are five times more likely to develop hepatocellular carcinoma. times that of healthy people. Obesity also increases the risk of developing many cancers. Obesity can cause cirrhosis and fatty liver disease. Smoking: Smokers have a higher risk of hepatocellular carcinoma than those who have never smoked.
2. Diagnosis of primary hepatocellular carcinoma

Các xét nghiệm viêm gan có thể chẩn đoán ung thư tế bào gan nguyên phát
2.1 Medical History Your doctor will start by asking about your medical history to rule out any potential risk factors.
2.2 Clinical Physical examination, pay attention to liver condition. They will then do a physical exam, focusing on the abdomen and any yellow in the whites of the eyes. These are both reliable indicators of liver problems.
2.3 Subclinical The subclinical diagnoses include:
Hematology, complete coagulation function. Liver and kidney function: ALT, AST, Billirubin, Albumin, BUN, Creatinine /blood. Hepatitis tests: AntiHBsAg, HBeAg, HBeAb, HBsAg, HCV-RNA, HBV-DNA, AntiHCV. AFP chest radiograph. Doppler ultrasound of hepatic vessels. Perform a contrast-enhanced CT scan of the abdomen (MRI of the abdomen if needed).

Hình ảnh chụp CT scan bụng
2.4 Definitive diagnosis Need one of the following three criteria:
There is pathological evidence that the primary hepatocellular carcinoma is . Typical image on contrast-enhanced abdominal CT or magnetic resonance imaging +AFP >400ng/ml. Typical image on CT scan of abdomen with contrast or MR + higher than normal AFP (400 ng/ml) + hepatitis B or C virus infection. Liver biopsy may be needed if clinician found necessary. All cases that do not meet the above criteria need a liver biopsy to confirm the diagnosis.
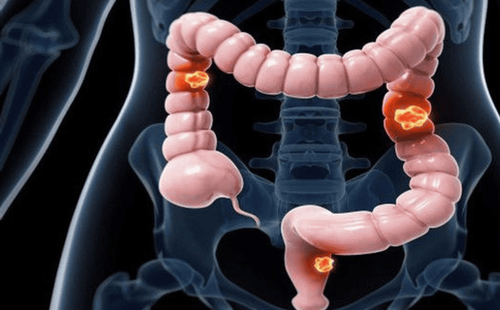
2.5 Differential diagnosis of liver hemangioma: Tumor gradually increases in luminosity from arterial phase to late phase, without drug drainage, AFP is normal. Intrahepatic cholangiocarcinoma: Uneven luminosity, no drug escape, elevated CA 19.9 cancer marker. Liver metastases of other cancers: There is an increased image of the border, the corresponding cancer markers are elevated, with the primary lesion. 2.6 Staging the disease Very early stage: Some cancer cells begin to gradually form tumors during this stage. There is one tumor smaller than 2cm, PS: 0, Child: A. Early stage: The tumor remains in the liver and has not spread to an organ or site. There is one tumor less than 5cm or less than 3 tumors, each less than or equal to 3cm, PS: 0, Child: A-B Intermediate stage: There are several small tumors existing in the liver or one tumor has arrived blood vessel. Large and multi-tumor, PS: 0, Child: A-B Advanced stage: There are many large tumors or one tumor has reached a major, major blood vessel. Tumor of any size portal vein thrombosis or extrahepatic metastases. PS: 1-2, Child: A-B Late Stage: The cancer has metastasized, which means it has spread to other parts of the body. Tumor can be any, PS: 3-4, Child: C Once the doctor has diagnosed and staged the cancer, the patient will begin treatment.
3. Treatment of primary hepatocellular carcinoma

Phẫu thuật cắt gan để điều trị ung thư tế bào gan nguyên phát
3.1 Surgery to remove the part of the liver containing the tumor Treating hepatocellular carcinoma with hepatectomy is a treatment that has the potential to completely eradicate HCC with a prognosis of 5-year overall survival from 50- 70%
Purpose of surgery:
Solve detected hepatocellular carcinoma Treatment of underlying diseases: Viral hepatitis, cirrhosis... Indications: PS 0-2, Child A, B, no distant metastasis, no portal hypertension.
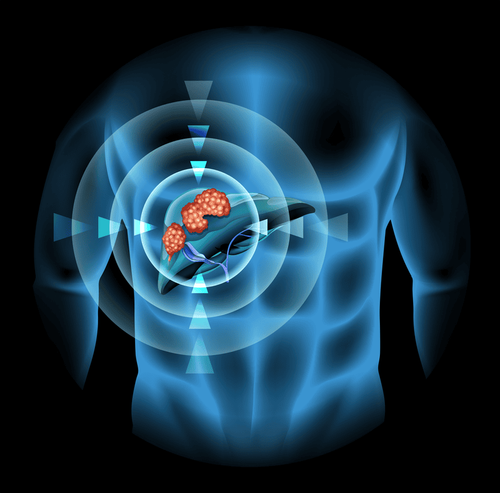
3.2 Tumor destruction in situ Radiofrequency ablation (RFA), absolute alcohol injection into the tumor. It is a thorough and effective treatment. These are minimally invasive interventions and most are performed percutaneously under ultrasound guidance with early thermal tumor destruction.
Indications:
The number of tumors is less than 3 and the tumor size is less than 3cm. A tumor smaller than 5cm is easier to reach. Tumors larger than 5cm with severe medical disease should be consulted. PS 0-2, Child A, B, No distant metastasis, comorbidities.
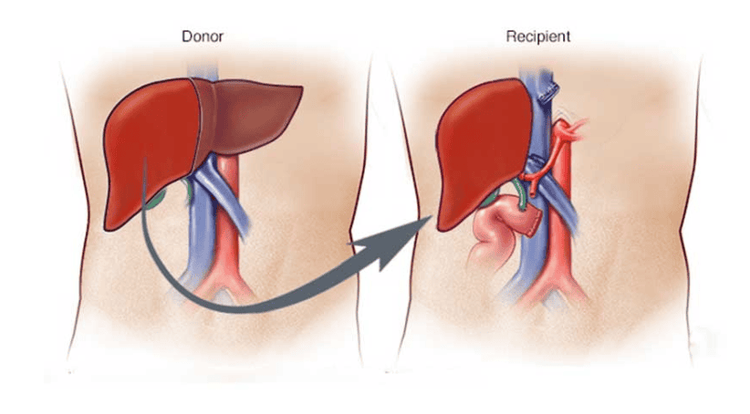
Phẫu thuật cấy ghép gan làm giảm nguy cơ ung thư tế bào gan trở lại
3.3 Cut off the blood supply to the tumor in combination with chemotherapy and radiation Radiation therapy is less effective in treating liver cancer and easily damages the healthy liver tissue around the tumor. Some new radiotherapy methods may be more effective, but are still in the process of completing research.
Systemic chemotherapy is a method of intravenous chemotherapy with little results, and only applied to cases of liver cancer that have been too indicated for treatment.
Indications:
Unresectable tumor, or multiple tumors in both lobes, may have small branch vein thrombosis. PS 0-2, Child A, B, no distant metastasis. 3.4 Liver Transplant Successful transplantation reduces the risk of hepatocellular carcinoma returning and restores normal liver function. However, the immune system may reject the new organ and attack it.
Indications: One tumor less than 5cm in size or no more than 3 tumors 3cm each.
Hepatocellular carcinoma is treatable with the development of current treatments. The earlier the disease is detected, the higher the chance of cure. And during treatment, patients should follow the doctor's instructions for the best treatment results.
To register for examination and treatment at Vinmec International General Hospital, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.