This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Huy Nhat - Department of Medical Examination & Internal Medicine - Vinmec Danang International General Hospital.
Nosocomial pneumonia caused by drug-resistant bacteria is increasing rapidly, causing difficulties in initial antibiotic treatment, increasing mortality, prolonging hospital stay and increasing treatment costs. Follow the article below to better understand the diagnosis and treatment of hospital-acquired pneumonia.
1. What is nosocomial pneumonia?
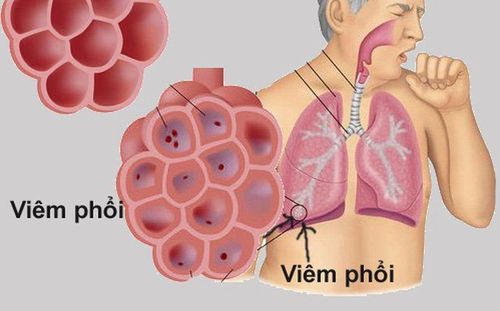
Hospital-acquired pneumonia is a common medical care-associated infection in the ICU and is the leading cause of death, accounting for 30%-70% of all hospital-acquired infections.Nosocomial pneumonia is pneumonia occurring 48 hours after admission with no prior respiratory symptoms or infection, and no new or progressive lesions on chest x-ray 48 hours prior to admission.
According to research in developed countries, nosocomial pneumonia accounts for 15% of all hospital infections, accounting for 27% of hospital infections in the ICU (data from the Center for Disease Control and Prevention). US Disease Control and Prevention 2003). Among hospital-acquired pneumonia, ventilator-associated nosocomial pneumonia (hospital pneumonia occurring after >48 hours of mechanical ventilation) accounts for 90%. Nosocomial pneumonia prolongs the hospital stay by about 6.1 days, which costs an additional $10,000 - $40,000 per case.
2. How is hospital-acquired pneumonia diagnosed?

However, the clinical presentation of pneumonia is often overshadowed by another pathology (eg, toxicity, drug allergy, atelectasis, pulmonary infarction, adult respiratory distress syndrome, congestive heart failure). , bronchitis). In addition, fluid aspirated into the lungs from the stomach also causes pneumonia, so it is difficult to distinguish from bacterial pneumonia.
2.2 Diagnosis According to the US Centers for Disease Control and Prevention, nosocomial pneumonia can be diagnosed by the following methods:
Percussion of the lung is cloudy or auscultated with crackles; New purulent sputum or change in sputum characteristics; Chest X-ray: Old infiltrates widen or new infiltrates appear, thickened lesions, pleural effusion; Positive blood culture; Isolation of pathogens from specimens obtained by tracheal aspiration, bronchoscopy or bronchial biopsy; Isolation of viruses or viral antigens from respiratory secretions; Positive IgM antibody or 4-fold increase in IgG antibody titer; There is histopathological evidence of pneumonia. For children under 12 months of age, diagnosis is based on the following symptoms:
Shortness of breath, rapid breathing, slow heart rate, cough; hear the lungs hear rales, rales; Increased secretions of the respiratory tract; Chest X-ray with new or progressive infiltrates, pulmonary consolidation, cavitation, pleural effusion; Sputum test: Gram stain: To guide antibiotic therapy while waiting for culture results. If < 10 epithelial cells and > 25 neutrophils are seen in a microfield, then there is a pulmonary infection; Sputum culture: Collect specimens by tracheal aspiration or bronchoscopy (protective brushing, bronchoalveolar lavage) for accurate results. Common microbial causes for hospital-acquired infections are as follows:
Bacteria: Blue pus bacillus, staphylococcus aureus, enteric bacteria, Klebsiella pneumoniae, Echerichia coli..., anaerobic bacteria; Influenza virus A, B; respiratory syncytial virus; Candida fungus.
3. Treatment protocol for hospital pneumonia

Currently, the treatment of hospital-acquired pneumonia is really difficult due to the increasingly serious situation of antibiotic-resistant bacteria and very few new antibiotics being invented.
In order to reduce mortality during treatment, the current approach is to treat with strong, broad-spectrum antibiotics, suitable from the beginning for the majority of hospital-acquired pneumonia caused by multi-resistant bacteria, patients with predisposing factors. high risk. After patients improve clinically and have microbiological results, antibiotic treatment will be narrowed down to avoid drug resistance and reduce costs.
3.1 Basis for antibiotic use Empiric antibiotic therapy: Apply to critically ill, high-risk patients with delayed diagnosis. Usage is based on the following grounds:
Criteria to define severe patients: The patient must be treated in the intensive care unit; With respiratory failure: Must mechanical ventilation or oxygen with concentration >35% to maintain SaO2 >90%; Pulmonary parenchymal lesions on x-ray are extensive with >1 lobe or cavernous; There are manifestations of severe sepsis: systolic blood pressure <90mmHg, diastolic blood pressure <60mmHg; must take vasopressors for more than 4 hours; oliguria (urine output < 20ml/hour); acute renal failure with indication for dialysis; Pneumonia appeared 5 days after admission. Having high risk factors for nosocomial pneumonia: Intubation or tracheostomy; Have a nasogastric tube; Patients over 70 years old; Have chronic lung diseases; Malnutrition; Comatose; Patients undergoing abdominal and chest surgery; Other conditions: Weakened immune system, prolonged hospital stay, respiratory viral infection, alcoholism, aerosolized antibiotics, diabetes mellitus, uremia. 3.3 How to use antibiotics Non-severe, early, low-risk: Use 1-2 types of antibiotics, specifically: 3rd generation Cephalosporins: Cefuroxim acetyl, cefotaxime, ceftriaxone; Or use beta-lactams and beta-lactamase inhibitors such as: ampicillin-sulbactam, ticarcilin-sulbactam, piperacillin- tazobactam; If allergic to penicillin: Use fluoroquinolone or clindamycin, azythromycin. Severe, late, high risk: Use 2-3 types of antibiotics, specifically: Aminoglycosides (gentamycin, tobramycin, amikacin) or ciprofloxacin; Antibiotics effective against blue pus bacilli: Ceftazidim, efoperazone, cefepim, piperacillin, ticarcillin, mezlocillin; or a betalactam (betalactamase inhibitor) such as ticarcilin-sulbactam, piperacilin-tazobactam; or imipenem, meropenem; or aztreonam; Vancomycin. If culture results are available, use antibiotics according to the instructions of the antibiogram.
Hospital pneumonia as well as respiratory diseases are examined and treated by a team of highly qualified and experienced doctors at Vinmec hospital. Including Master, Doctor Nguyen Huy Nhat with many years of experience in the field of respiratory disease treatment at Hue Central Hospital, Hoan My General Hospital, .. before being a doctor of General Internal Medicine Department. Vinmec Da Nang International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.