This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Huy Nhat - Department of Medical Examination & Internal Medicine - Vinmec Danang International General Hospital.
Bronchiectasis was a common disease in the pre-antibiotic era and easily led to disability and death. However, at this time, the incidence has become rarer thanks to the effective use of antibiotics for respiratory infections and immunostimulating drugs in children against diseases such as measles and whooping cough. ,...
1. What is bronchiectasis?
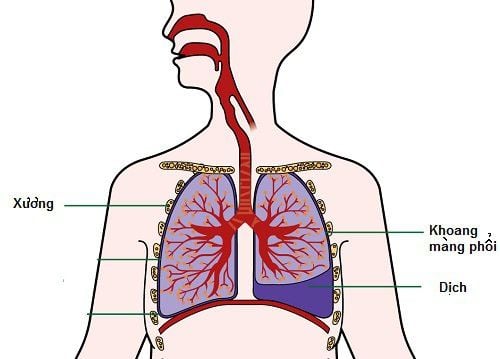
Bronchiectasis is a permanent and irreversible dilation of one or more bronchi with destruction of the bronchial wall structure, causing symptoms such as cough, sputum production, and recurrent respiratory infections. The bronchioles are irreversible and are often associated with other diseases. Bronchiectasis is divided into the following types: sacral bronchiectasis, cylindrical bronchiectasis and rosary bronchiectasis.Bronchiectasis can be congenital, inherited or acquired, can be focal and limited to only one or one lobe of the lung, but can also extend to multiple lobes on one or both sides lung .
2. How is bronchiectasis diagnosed?
2.1 Definitive diagnosis To definitively diagnose bronchiectasis should be based on both clinical and subclinical symptoms of the patient. Clinically, the patient's symptoms will include functional, physical and subclinical symptoms.Functional symptoms:
Persistent productive cough: this is a very important symptom. The patient may cough up green or yellow pus-filled sputum, which may contain a little or a lot of blood (over 150ml/day). If the sputum is left to settle, it will be divided into 3 layers, including the upper foam layer, the pus-filled mucus layer in the middle and the cloudy pus at the bottom. Some patients also have no cough or dry cough due to dry bronchiectasis in the upper lobes. Coughing up blood: In some cases, it can be the only symptom of the disease, coughing up blood again and again, lasting for many years. The degree of hemoptysis may be less or more, if the large amount is 500ml/day, it may be accompanied by acute respiratory failure. Shortness of breath: this is a symptom that often appears late, there may be bruising of the lips and extremities, a complication of respiratory failure due to diffuse damage to the lungs. Fever: symptoms often appear after respiratory infections, when fever is often accompanied by increased sputum or change in sputum color.

Trong một số trường hợp, ho ra máu có thể là triệu chứng duy nhất của bệnh
Auscultation of the lungs is mainly moist, crackles. Hissing, snoring can only be heard in the acute phase, there may be contractile condensate syndrome when atelectasis occurs. The sign of cupped fingernails is seen in patients with repeated, persistent bronchial superinfections. Symptoms of cor pulmonale such as: leg edema, hepatomegaly, distended neck veins,... Subclinical symptoms:
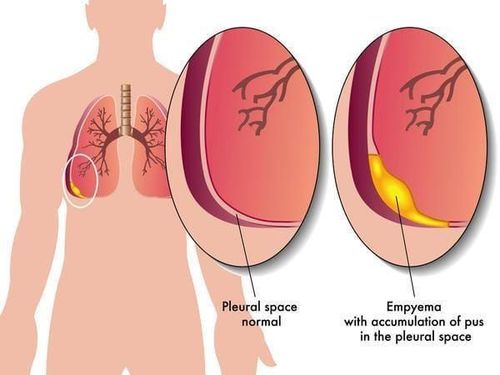
Chest X-ray: signs suggestive of bronchiectasis can be seen such as: The bronchial walls create parallel lines, the volume of the lobes expands, the bronchi shrink or have bright foci like a honeycomb image. High resolution computed tomography (CT scan) scan: this is a gold test to diagnose bronchiectasis with signs such as the diameter of the bronchi being larger than the accompanying artery, the bronchi not becoming smaller in diameter. as specified. 2.2 Differential diagnosis Usually a differential diagnosis is required when the patient has not been subjected to computed tomography. Differential diagnosis is often with some of the following diseases:
Lung abscess: relatively difficult to distinguish when bronchiectasis is accompanied by acute superinfection. Pulmonary tuberculosis. Air cysts in superinfected lungs: differentiated by computed tomography.
3. How to treat bronchiectasis?

Kháng sinh được lựa chọn có thể dùng cho đường uống hoặc tiêm tùy thuộc vào mức độ nặng của bệnh nhân
3.1 Treatment of bronchial superinfection The antibiotic of choice can be given orally or by injection depending on the severity of the patient. Bronchodilators for patients with superinfection are usually 2nd generation Cephalosporin antibiotics combined with Aminoglycoside antibiotics. Some antibiotics that can be used to replace are Penicillin or if beta-lactamase-producing bacteria are suspected, then Penicillin G can be replaced with Amoxicillin + Clavulanic Acid or Ampicillin - Sulbactam. The usual duration of antibiotic use is 1-2 weeks but may be longer for severe cases of bronchiectasis, drug-resistant bacteria. Instruct the patient to cough up sputum, palpate the chest or drain in a position to avoid backlog causing superinfection. 3.2 Treatment of bronchospasm Conducted when the patient has difficulty breathing, the lungs hear rales, rales. Medications used may be beta-2 agonists, anticholinergics, or a combination of both. 3.3 Treatment of hemoptysis If coughing up a small amount of blood, you can lie down, eat liquids and take cough suppressants. If hemoptysis is moderate, the above regimen can be used in combination with Transamin and Morphine (with caution in chronic respiratory failure). If hemoptysis is severe and severe, it is necessary to use morphine, vasoconstrictor drugs, combined with intravenous fluids, blood transfusion to supplement circulating volume. Some cases of blood clots causing bronchial obstruction require blood sputum aspiration, endotracheal intubation or tracheostomy to remove. All cases of moderate or higher hemoptysis should be treated with antibiotics to prevent infection. Doctor Nguyen Huy Nhat has many years of experience in the field of respiratory disease treatment at Hue Central Hospital, Hoan My General Hospital, .. before being a doctor of General Internal Medicine Department of National General Hospital. Vinmec Danang International.
For detailed advice about the disease, please come directly to Vinmec health system or book online HERE.
MORE:
Is bronchiectasis contagious? Bronchiectasis dangerous? Notes in the use of bronchodilators