This is an automatically translated article.
Asthma in children is a common respiratory disease caused by allergic factors. Diagnosing and detecting bronchial asthma in children and timely treatment will help control the disease effectively.
1. Overview of bronchial asthma in children
Childhood bronchial asthma is a chronic inflammation of the airways caused by irritating factors such as weather, dust, allergens, ... that increase bronchial sensitivity and cause symptoms such as cough , wheezing, rapid breathing, chest pain. However, there are some cases (children under 2 years of age) with only mild and transient wheezing, and in some cases, there may be no symptoms until the child is 6 years old.
Asthma in young children can cause many relapses. If not diagnosed and treated early, the disease can leave many sequelae of the respiratory tract later.
2. Diagnosis of bronchial asthma in children
Diagnosis of childhood asthma includes 3 steps as follows:
Step 1: History of the child Step 2: Clinical examination Step 3: Other methods of assessing respiratory function and testing
2.1 History of the child
Children with a history of repeated symptoms such as:
Cough Wheezing Shallow, rapid breathing Chest pain Symptoms of asthma in young children often occur at night with a more severe degree, can be wake the child up. The disease can get worse when children are infected with viruses, are exposed to allergens such as pollen, pet dander, mold, dust, changes in weather, and strenuous exercise such as sports.

Hen phế quản trẻ nhỏ
Asthma in children is often underdiagnosed, especially when the child has an accompanying respiratory infection but is not treated appropriately. Therefore, it is important to consider the diagnosis of asthma in young children with frequently repeated diagnoses such as:
Allergic bronchitis Wheezing Bronchitis Asthmatic bronchitis Recurrent pneumonia Recurrent bronchiolitis Causes Children with bronchial asthma are often underdiagnosed due to the following factors:
Children with tracheoesophageal fistulas Children with foreign bodies in the airways Children with congenital heart disease with pulmonary hypertension Children with gastroesophageal reflux bronchial TB Children with tuberculosis lymph nodes or mediastinal tumors Immunocompromised children Children with bronchopulmonary dysplasia Diagnosis of asthma in young children should also be based on suspicious signs that are not asthma, such as:
The child has cyanosis, vomiting when eating or feeding Child not gaining weight Child with drumstick fingers Child not responding to appropriate asthma treatment

Trẻ không tăng cân có thể là dấu hiệu của bệnh hen suyễn
2.2. Clinical examination
Clinical examination needs to quickly assess the severity of asthma attacks in young children to promptly handle:
Mild asthma: The child is still awake, only having difficulty breathing when exertion, can still lie down. The child is breathing rapidly but without chest constriction. SpO2 > 95%. Moderate asthma: The child is awake, has obvious symptoms of dyspnea, may not be able to lie down. The child is breathing rapidly and has chest indrawing. SpO2 measured is in the range of 92 - 95%. Severe asthma: Children struggle, are excited and constantly find it difficult to breathe, cannot sit, have to lie down with their heads high. Asthma in children causes rapid breathing and chest constriction. SpO2 <92%. Critical asthma: The child is cyanotic, comatose, slow breathing or has an asthma attack. The alveolar murmurs are reduced or may be inaudible. SpO2 <92%.

Kiểm soát và điều trị hen phế quản trẻ nhỏ cần tránh tiếp xúc với khói thuốc lá
2.3 Methods of assessing respiratory function and some other tests
Methods of assessing respiratory function and testing used to diagnose asthma in young children include:
Spirometry: Measure respiratory function with indexes FEV1, FVC, ratio FEV1/FVC. The results showed that the obstructive syndrome responded to beta 2 stimulation if FEV1 decreased, FEV1/FVC ratio <0.8, after taking bronchodilators, FEV1 increased to 200ml or 12%. Peak flow measurement: Measure and monitor the child's peak expiratory flow (PEF) from 1 to 2 weeks when the child has asthma symptoms but spirometry shows normal results. In addition, this index also helps assess the severity of asthma in children so that the doctor can recommend appropriate treatment. Measure exhaled NO: This is a non-invasive biomarker test indicated for children with inflammation when wheezing recurs. Measurement of NO is often elevated in asthmatic patients or during acute asthma attacks, and decreases when patients are treated with inhaled or oral corticosteroids. This test has an accurate diagnosis rate of up to 80% of cases of asthma.
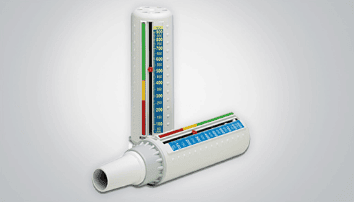
Sử dụng đo lưu lượng đỉnh kế để đánh giá chức năng hô hấp
2.4 Diagnostic criteria for bronchial asthma in children
Diagnosis of childhood bronchial asthma is based on the following 5 criteria:
The child has frequent recurrences of cough and wheezing After ruling out other causes of cough and wheezing Child has asthma risk factors Yes response to bronchodilators Clinical examination and diagnostic tests show that the child has asthma
3. Asthma in children and how to treat
3.1 Drug treatment
Treatment of asthma in children with medication includes reliever and preventer:
Reliever drugs include: short-acting beta 2 agonists (Ventolin injection or oral, Bricanyl oral), Ipratropium bromide ( Atrovent, Combivent), Oral or injectable corticosteroids (for short-term use), Theophylline injectable, Magnesium sulfate. Preventative medications include: inhaled corticosteroids - ICS (beclomethasone, budesonide, fluticasone), long-acting beta-agonists (formoterol, salmeterol for children older than 5 years), Leukotriene modifiers (montelukast, zafirlukast), delayed-release Theophylline , Anti-IgE. Factors that can make childhood asthma worse:
Children with rhinitis or sinusitis Children with gastroesophageal reflux disease Children who are allergic to medications If treated appropriately, the above conditions can be reduce the frequency and severity of asthma attacks.
Viêm xoang làm trầm trọng thêm các triệu chứng hen phế quản của trẻ em
3.2 Controlling factors in the treatment of asthma in children
Treatment of bronchial asthma in children requires controlling factors that contribute to asthma exacerbation by:
Limiting exposure to the environment, people who are sick with flu, proactively preventing influenza with influenza vaccination . Avoid exposure to environments with a lot of cigarette smoke. Regularly clean the house, clean bed. Avoid contact with pets and insects.
3.3 Evaluation and monitoring of treatment and control of asthma in children
Treatment of asthma in children requires periodic follow-up visits to check treatment adherence, increase or decrease drug dose (if necessary) and evaluate ACT and CACT.
Uncontrolled bronchial asthma: Take the child for re-examination every 2 weeks. Partially controlled asthma: Take the child for re-examination once a month. Asthma is thoroughly controlled: Take the child for re-examination every 3 months.

Trẻ em mắc bệnh hen phế quản cần được đi khám sức khỏe định kỳ
3.4 How to manage asthma attacks in children at home
When children have symptoms of cough, wheezing, tired breathing, give them 2 sprays of Salbutamol 100 micrograms (for young children, 4 sprays need to be combined with babyhaler) with a dose of 20 minutes/time in the first hour if the child has not cut it. bout. After that, assess the ability to respond to asthma attacks in young children:
Children respond well if they stop breathing tired and manage to relieve asthma attacks lasting 4 hours: Continue to spray Salbutamol 100 micrograms for children 3 - 4 hour/time in 1-2 days. Parents and caregivers contact the doctor to take the child to the doctor. Children with incomplete response, only moderate asthma: Let the child continue to inhale salbutamol every 1-2 hours, use oral corticosteroids and take the child to the doctor at the earliest time of the day. Children who do not respond to drugs and still have symptoms of shortness of breath: For children to continue to inhale Salbutamol in combination with Ipratropium, use oral corticosteroids. The child was rushed to the emergency room. Asthma in children needs to be detected early to control and treat the disease. During treatment, it is necessary to pay attention to comply with the treatment regimen of the doctor, take the child for regular check-ups.
Vinmec International General Hospital is the address for receiving and examining respiratory diseases that infants and young children are susceptible to: viral fever, bacterial fever, respiratory infection, asthma management, pneumonia in children, .... With modern equipment, sterile space, minimizing the impact as well as the risk of disease spread. Along with that is the dedication from the doctors with professional experience with pediatric patients, making the examination no longer a concern of the parents.
Especially now, to improve service quality, Vinmec also deploys many medical services, including the Asthma Screening Package to help screen and detect the disease early to promptly control and treat the disease. performing clinical examination, taking medical history, measuring respiratory function, otolaryngology examination, screening for bronchial asthma.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.