This is an automatically translated article.
The article was written by MSc Vu Ngoc Thang - Urology Surgeon, Vinmec Times City International General Hospital.Bladder cancer originates from many types of cells, in which the rate of bladder carcinoma accounts for the absolute majority (98%), the highest rate among urinary tract cancers and the second most common in genitourinary tract cancers. The male/female ratio is 2.7/1 and is more common in whites than blacks. If diagnosed early and treated promptly, the 5-year survival rate for bladder cancer can be as high as 80%.
1. Diagnosis of bladder tumor
1.1 Definite diagnosis 1.1.1 Clinical Unexplained hematuria, intermittent hematuria. Low back pain or palpable tumor in the late stage. 1.1.2 Subclinical Diagnostic Imaging
Ultrasonography: shows tumor arising from the wall, protruding into the bladder lumen, possibly with a stalk. Assess the location, size of the tumor, can assess the invasion into the bladder wall. CT-scanner: allows to evaluate the size and location of the tumor, the extent of invasion into the bladder wall and surrounding tissues, and search for metastatic lymph nodes in the pelvic fossa. metastases in lymph nodes, liver, etc. MRI (if necessary): assess tumor location, size, boundaries and invasion level of the tumor. Helps to detect thrombus in the renal vein, vena cava, differentiate metastatic lymph node and blood vessel. Cystoscopy and biopsy: this is the optimal method to confirm the diagnosis of bladder tumors, and allows biopsy of the tumor to determine the invasiveness and malignancy (cell differentiation) of the tumor. from which appropriate treatment is indicated. Blood test
Complete blood count: Red blood cells, hemoglobin may decrease if hematuria is severe and prolonged. Biochemical tests: little change. Hypercalcemia is caused by cancer secreting parathyroid hormone-like substances, or metastases to bone, stimulating osteoclasts to function. Urine test
Red blood cells, white blood cells positive. Immunohistochemical staining: Immunohistochemical staining of bladder cancer tissue is carried out to detect cancer markers. Some studies show that markers BrdU-LI, cyclin D1, EMT... increase in bladder cancer. Other tests
Plain slant chest x-ray identifies lung metastases. Bone scan: Find bone metastases. This is not a routine indication, only done when there are signs of bone pain. PET/CT scan: Detect metastasis.
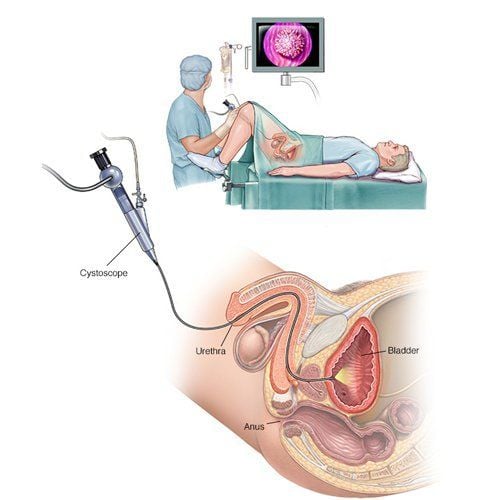
Soi bàng quang và sinh thiết là một trong các phương pháp tối ưu giúp chẩn đoán u bàng quang
2. Stage division
2.1 TNM division 2.1.1 T (tumor: tumor) + Tx: Unidentified tumor.
+ T0: Undetectable primary tumor.
+ Tis: Flat tumor in the mucosa.
+ Ta: Non-invasive papillary cancer, localized in the mucosal layer.
+ T1: Cancer invades the basement membrane.
+ T2: Cancer invades muscle layer.
T2a invades the superficial muscle layer. T2b invades the deep muscle layer. + T3: Tumor invades the tissue layer adjacent to the bladder.
T3a Small tumor in the fatty layer around the bladder (microscopically identified). T3b Tumor is large outside the wall of the bladder (macroscopically identifiable). + T4: Tumor invades nearby organs.
T4a invades the prostate, ureters, uterus, or vagina. T4b invades the abdominal wall, the pelvic wall. 2.1.2 N (Nodules: lymph nodes) Nx: No metastatic lymph nodes are identified. N0: No lymph node metastasis. N1: Metastasis to 1 lymph node <2cm in size. N2: Metastasis to one or more lymph nodes 2-5 cm in size. N3: Metastasis to one or more lymph nodes > 5cm in size. 2.1.3 M (metastase: distant metastasis) Mx: No distant metastasis can be identified M0: No metastasis M1: With distant metastasis According to this division:
Superficial bladder cancer is tumor in stages Tis, Ta, T1 Deep bladder cancer is a tumor in stages T2a-b, T3a-b, T4a-b 2.2 Staging Based on the depth of invasion of the bladder wall according to Jewett (1946):
Stage stage A: Invasion of submucosa Stage B: Invasion of muscle layer Stage C: Invasion of the entire bladder wall Stage D1: Invasion of adjacent organs
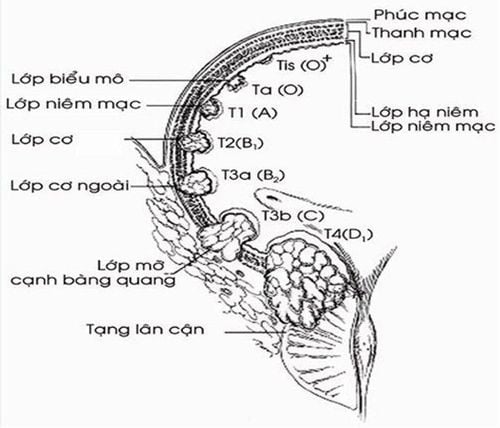
Hình ảnh mô tả độ sâu xâm lấn thành bàng quang theo Jewett (năm 1946)
3. Surgical treatment
3.1 Treatment of bladder cancer that has not invaded the muscle layer 3.1.1 Transurethral endoscopic cystectomy laparoscopic transurethral resection is the method of first choice in the treatment of bladder cancer in pTa or pT1 stage. This is a cure for many cases. Applied to solitary tumor or 2-3 tumors, tumor size ≤ 3.
3.1.2 Prophylaxis against recurrence after laparoscopic cystectomy After transurethral endoscopic resection for bladder tumor, rate The recurrence rate is usually quite high. Injecting antibiotics that inhibit mitosis (Mytomycine C, Doxirubicine) or pumping BCG into the bladder can help limit the recurrence of bladder tumors.
Mytomycine C pump is indicated for bladder tumors with mild or moderate malignancy. BCG pump is indicated for cases of high malignancy (grade 3) or pT1 bladder carcinoma.
3.1.3 Partial cystectomy Partial cystectomy is indicated for cases where endoscopic transurethral resection cannot be performed. Tumor in bladder diverticulum. The risk of tumor spreading into the peri-bladder tissue during surgery is very high.
It is possible to combine ligation of the two internal iliac arteries to temporarily reduce the feeding of the tumor.
3.1.4 Total cystectomy alone Indications for total cystectomy in the treatment of non-muscle-invasive bladder carcinoma are rare. Tumor gas occupies almost the entire surface of the bladder, it is not possible to perform transurethral endoscopic resection or partial cystectomy. In addition, if the recurrence is many times even though the number is small, the malignancy is high (Grade 3).
Total cystectomy combined with urine flow measures: plugging the ureter into the intestine, draining the ureter to the skin, rebuilding a new bladder.
Surgical methods: Open surgery, laparoscopic surgery, Robot surgery.
3.2 Treatment of bladder carcinoma that has invaded the muscle layer 3.2.1 Radical total cystectomy Is a rather heavy surgery, including dissection of obturator iliac lymph nodes, total removal of bladder, prostate, sac. crystal, shiny. In women, the entire uterus and two ovaries and fallopian tubes are removed.
Can be combined with different urine diversion techniques.
Indicated when bladder carcinoma has invaded the muscular layer but not outside the bladder wall (pT2, pT3, N0, M0), no lymph node and distant metastasis.
Only perform this technique in patients in good condition, with a survival time of more than 10 years.
Surgical methods: Open surgery, laparoscopic surgery, Robot surgery.
3.2.2 Total cystectomy Indicated when bladder carcinoma has invaded the muscular layer but not outside the bladder wall (pT2, pT3, N0, M0), no lymph node metastasis and no metastasis distant. The condition does not allow radical cystectomy or the prognosis for survival is not more than 10 years
Total cystectomy combined with measures for urine flow: inserting the ureter into the intestine, draining the ureter to the skin, new bladder reconstruction.
Surgical methods: Open surgery, laparoscopic surgery, Robot surgery
3.2.3 Partial cystectomy Indicated when bladder cancer has invaded the muscle layer, but general condition does not allow radical cystectomy. apartment.
Need to be combined with combined chemotherapy and radiation methods.
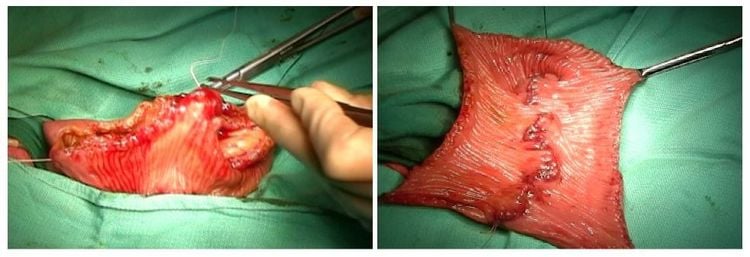
Tạo hình bàng quang mới bàng quai ruột
4. Complications and treatment
4.1 In surgery Acute intraoperative bleeding: Management depends on the cause. Injury to internal organs Perforation of colon, rectum: Switch to open surgery to treat according to lesions. Injury to the jejunum is very rare: Treatment depends on the lesion. Injury to the uterus: Treatment depends on the damage. 4.2 After surgery Bleeding: Resuscitate, if not, switch to surgery to stop bleeding. Accumulation or residual abscess in the abdomen: Accurately determine the location and size of the collection or abscess by ultrasound or computed tomography. + Fluid collection, small abscess < 5cm. Superficial aspiration can be performed under ultrasound guidance.
+ Fluid collection, large deep abscess must drain or surgically clean the abscess.
5. Care and follow-up after surgery
Remove abdominal drainage after about 3-5 days. Monitor general status, vital signs, urine, electrolytes after surgery.
6. Health counseling and education before and after the technique
6.1 Health counseling and education before performing the technique Complete the health education sheet for patients and relatives. Advice on the treatment methods, the method of choice with the advantages and disadvantages of the method. The normal manifestations can be seen after surgery: Postoperative movement. 6.2 Counseling, health education after performing the technique Surgical methods, changes if any compared to the original plan. Symptoms that need to be reported to the doctor. Re-examination time. The article references the source:
Vu Le Chuyen (2012), “Overview of bladder cancer”. Do Truong Thanh (2007), “ Bladder Cancer”, Urological Pathology, Medical Publishing House, (pages 399 – 412). NCCN Guidelines Insights Bladder Cancer, Version 5.2018. European Association of Urology Guidelines 2019. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out. with comprehensive and professional medical examination, consultation and treatment services; civilized, polite, safe and sterile medical examination and treatment space.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
MORE:
How to detect bladder cancer early? Stages of Bladder Cancer Treatment Prognosis in Bladder Cancer