This is an automatically translated article.
The article was consulted with Specialist Doctor I Huynh Kim Long - Emergency Resuscitation Doctor - Emergency Resuscitation Department - Vinmec Danang International General Hospital.A coma signals a critical condition that occurs due to abnormal changes in the brain's ability to respond to activities in the body's organs, which are mainly caused by trauma and metabolic diseases.
1. What is a coma?
Coma is a disorder of consciousness due to the occurrence of diffuse trauma to the two hemispheres of the brain in combination with the afferent reticular system or affecting the reticular activating system.2. Causes of coma
2.1 Anatomical damage Some common anatomical injuries can cause coma such as:Head trauma: Traumatic brain injury, intracranial hematoma Complications after head injury: Subdural hematoma Stroke Brain: Brain hemorrhage, cerebral infarction... Epilepsy 2.2 Metabolic disorders Some metabolic disorders can lead to coma such as:
Diabetes causes high or low blood sugar Poisoning: alcohol, sleeping pills ... Hypopituitarism Hyperthyroidism or hypothyroidism

3. Clinical diagnosis of coma
3.1 State of consciousness Loss of consciousness: Loss of consciousness, memory loss, loss of voice, loss of posture.Loss of consciousness has 4 levels: Gloomy, confusion, somnolence and coma
3.2 Respiratory characteristics Respiratory disorders Deep tachypnea Rapid shallow breathing Apnea Apnea Cheyne - Stokes Disorder Circulatory: Tachycardia, hypertension, hypotension 3.3 Pupils The function of the pupils is influenced by both sympathetic and parasympathetic nervous systems. Changes in pupillary response and diameter are important in the monitoring of coma. Some features of the pupil and associated brain lesions, include:
Miosis: Miosis is an early sign of damage to the medial brain region. Loss of reflexes on one side: Injury to III nerve ipsilateral Loss of reflexes: midbrain injury

The two eyeballs are brought out: Shows a relatively deep coma because the muscle tone of the dilated eyeball is stronger than that of the adductor muscle. Eyeball pendulum, eyeball wandering (the phenomenon of the eyeball swinging back and forth without rhythm): Brain stem damage. Epilepsy-type nystagmus: A phenomenon in which both eyelids and eyeballs vibrate. Simple nystagmus (the phenomenon of rolling eyes on all sides): Third ventricle damage. Eyeball bowing (eyeballs go down sharply, slowly up): Injury to the pons. Head-eye reflex: A phenomenon where the eyeball is reversed with the direction of the head (head turning, head flexion, head tilt). Eyeball examination is not performed in people with spinal cord injuries and increased cranial pressure.
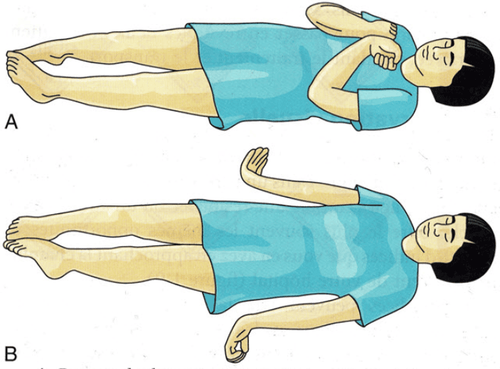
3.5 Movement and reflexes Motor
The goal of motor testing is to observe and determine whether the patient has natural, conscious or automatic movement. This is a difficult test to evaluate accurately because it depends on many factors such as the level of stimulation, the location of the stimulus, the patient's subjective response, etc. Motor assessment is mainly based on the main upper extremity responses:
Upper extremity retraction, adduction: loss of cortex Upper limb extensor, adduct, and pronation (twisting): Brain loss No motor response. Loss of cortex or brain is not significant anatomical damage. Loss of movement may just be a metabolic disorder. To confirm, the doctor must also look for convulsive movements, muscle twitches, signs of flapping wings, shaking hands.
Increased tendon reflexes have a high probability of deep coma. The Babinski sign (+) often co-occurs with limb paralysis. Eye-ear reflex
Eye-ear reflex is determined by pumping cold water into the ear, but the tympanic membrane must be checked for integrity. Tilt head to 30°, drain water into ear, use syringe without core. In coma, if the peripheral and interocular lines are intact, the eye responds gradually toward the water pump.
Turn your head to the right: Both eyes look to the left. Turn your head to the left: The eyes look to the right. Tilt your head back: Eyes look down. Bend your head forward: Eyes look to the left. Pump cold water into both ears: Eyes look upwards.
4. Subclinical diagnosis of coma
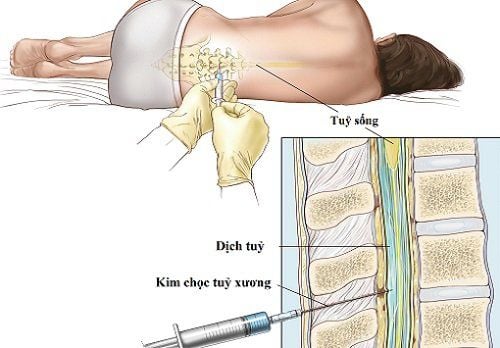
The subclinical indications in the diagnosis of coma are very diverse as well as the causes leading to coma. For traumatic coma, CT, MRI, and X-ray tests are important. As for the coma due to metabolic disorders, the cerebral angiography, blood biochemistry, etc. play an important role. In addition, the tests have their own contraindications, so depending on the diagnosis, the appropriate type of test is selected. Overall, the following tests are the most commonly used in the diagnosis of coma:Craniocerebral imaging. Capture the bottom of the eye. Cerebrospinal fluid puncture: Lumbar puncture plays an important role in the diagnosis of meningitis. In contrast, this test is unnecessary in traumatic brain injury and should not be performed in stroke.
5. Coma management
Respiratory resuscitation Respiratory resuscitation is the first thing that needs to be done to maintain life and brain function. Tasks to do for respiratory resuscitation include: Open airway, provide oxygen, provide respiratory support, intubation, etc. Use sedation for mechanically ventilated patients with increased intracranial pressure.Circulatory resuscitation The amount of oxygen supplied to the brain depends on the blood supply to the brain. Depending on the cause of the hemodynamic disturbance, give fluids or use cardiac drugs. In particular, for hypertension with cerebrovascular accident, attention should be paid to maintaining hemodynamic stability.
Glucose supply Hypoglycaemic coma has the potential to cause irreversible complications if not treated promptly. For diabetic patients who are comatose of unknown cause, it is necessary to do a glucose injection test (slow intravenous injection of 50ml glucose 30 - 50%) after taking blood for blood sugar test.

Electrolyte and Osmotic balance Water and sodium balance are the most basic electrolyte balance measures to be taken, but too rapid recovery should be avoided. In a coma, osmolality will be increased, if hypotonic fluids are given too quickly with insulin, it can cause water intoxication and cerebral edema.
Many factors affect water and electrolytes such as renal failure, increased ADH, dehydration, salt loss, extrarenal, diuretic, infusion of osmotic solutions, feeding, etc. Therefore, doctors need to calculate carefully before proceeding to provide electrolytes to the patient.
Acid-base balance Acid-base balance is similar to water-electrolyte balance. However, it should be noted that balancing metabolic acidosis too quickly with alkaline substances can cause temporary respiratory depression, making CSF more acidic. Thereby increasing PaC02, it is difficult to adjust immediately with bicarbonate.
Anti cerebral edema If there is a progressive neurological process accompanied by a decrease in consciousness, brain edema must be considered and treated immediately. If intracranial pressure cannot be directly measured, the physician should make a diagnosis of cerebral edema based on clinical experience and risk factors for cerebral edema. In the treatment of cerebral edema, anticoagulation should not be used because it causes bleeding at the lesion site.

The diagnosis and treatment of coma should be done in a timely manner, according to the correct procedure to avoid injury and ensure the safety of the patient's health.
Coma signals a critical condition that can lead to respiratory failure, death, so this is an emergency situation that requires urgent diagnosis and treatment.
Vinmec International General Hospital has a team of doctors and emergency nurses at the Emergency Department who are highly trained and methodical, able to receive and urgently handle severe cases. Continue to coordinate monitoring and treatment in the ICU with modern machines such as: PiCCO invasive hemodynamic probe, ECMO (artificial heart-lung) machine, Prismaflex continuous dialysis machine, GE ventilator Carescape R860...
In addition, with a system of modern facilities and medical equipment (CT 640, MRI 3.0 tesla...) combined with a team of specialists with many years of experience in the field of health care. With neurological conditions, stroke can be diagnosed early and treated quickly.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: slideshare.net