This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.In daily diagnosis, we sometimes encounter endoscopic diagnoses of diaphragmatic hernia, in some severe cases requiring surgery. So what is a diaphragmatic hernia? Is this disease dangerous? How is this disease diagnosed? This article will tell us the above information.
1. What is diaphragmatic hernia?
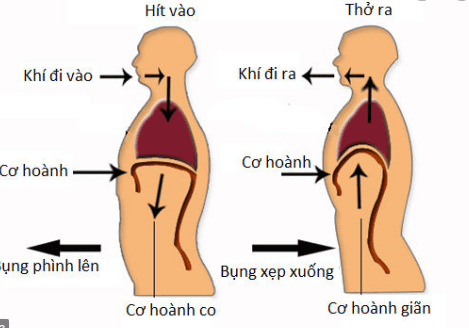
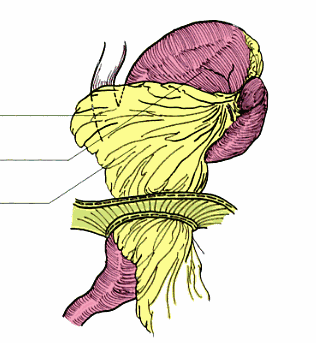
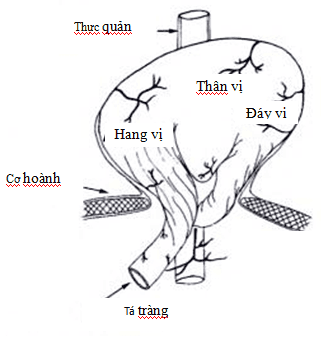
The diaphragm is a muscle, separating the abdominal cavity from the thoracic cavity, in this muscle, there are holes, slits, and recesses for the structures between the chest and abdomen to communicate with each other.Diaphragmatic hernia is a defect or opening in the diaphragm that allows abdominal organs to move into the chest cavity.
A hiatal hernia occurs when the stomach or other organs protrude into the mediastinum through the esophageal opening of the diaphragm.
This is a common disease in medical practice.
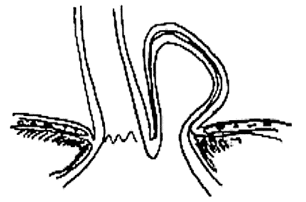
(I) hiatal hernia with short esophagus (II) paraphrenic hernia (III) ) diaphragmatic hernia does not include these 2 types. Recently, diaphragmatic hernias are classified into 4 types:
Type I with esophageal-stomach junction sliding into the mediastinum, pulling the stomach below it, this type accounts for 95% of hiatal hernias, usually asymptomatic symptoms or signs of gastroesophageal reflux disease. In type II, the gastroesophageal junction remains in place, but part of the fundus slips into the paraesophageal mediastinum, which is rare, <1% of all hernias. Type III hiatal hernia (mixed hernia), is characterized by both the fundus and the gastroesophageal junction in the mediastinum. Type IV is a wider hernia than type III with hernia visceral colon, spleen, and liver located in the thorax. Another rare type of hiatal hernia is a paraphrenic hernia, in which the stomach herniates through a small defect in the diaphragm, lateral to the left ulnar, anterior to the diaphragm.
2. Classification of diaphragmatic hiatus hernia
Type I (also called sliding, concentric, or axial): With an esophageal junction the stomach slides into the mediastinum, pulling the stomach below it.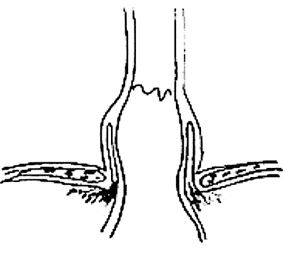
Type II, III, IV hiatus hernias are also called paraesophageal hernias.
Giant diaphragmatic hernia: depending on the definition of the authors, when the diameter of the hernia hole is larger than 5 cm, or more than 1/3 of the stomach is located in the thorax.
3. Frequency of hiatal hernia
The frequency of diaphragmatic hernias in the general population is difficult to determine, as the majority of patients with hernias are asymptomatic. The frequency of type I hernia is 7 times higher than that of type II, some documents record that about 90% of diaphragmatic hernia is type I, about 10% is type II hernia.The age distribution is significantly different between type I and type II. The frequency of diaphragmatic hernias increases with age, from 10% of people under 40 years of age to 79% of people over 70 years of age. The mean age of diaphragmatic hernia is 61 years old, recently 48 years old. Type II hernias usually occur in women, with a female/male ratio of 4/1.
4. Favorable factors of diaphragmatic hernia
Muscles (including the diaphragm, which contains the two pillars of the diaphragm) are weak and have reduced elasticity (acquired hernias in the elderly). Diaphragmatic cleft defect (congenital hernia in young people). Increased pressure in the abdominal cavity (ascites, women, obese people, people with chronic constipation...) Chronic esophagitis (fibrosis of the longitudinal muscle layer, leading to a shortened esophagus).5. Symptoms of diaphragmatic hernia
There was no clear relationship between hernia orifice size and clinical symptoms. A large hernia may be asymptomaticPatients with hiatal hernia may have one of the following three clinical manifestations:
Silent (most cases), the patient is discovered incidentally through a medical examination or because of another illness. Symptomatic (reflux esophagitis, or symptoms of paraesophageal hernia). Complications (gastric torsion, gastric necrosis). Possible symptoms:
Epigastric pain or pain just behind the sternum Burning behind the sternum Fullness, indigestion Vomiting, vomiting blood Chest pain Shortness of breath Choking Left lower quadrant pain...
6. Physical symptoms of diaphragmatic hernia
Usually nothing is detected. Physical symptoms, if present, are also of little diagnostic value. The patient may have mild anemia, general obesity, ascites... Bowel sounds can be heard in the chest, percussion area is opaque in the chest.7. Diagnostic procedures for diaphragmatic hernia
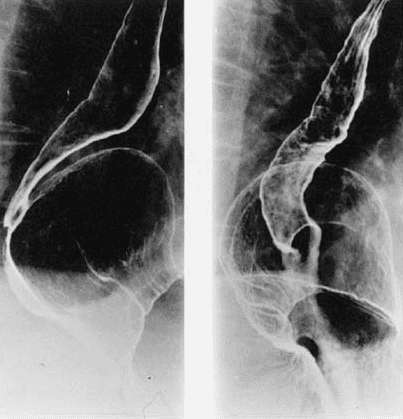
7.1. Straight, lateral chest radiograph: Most cases of diaphragmatic hiatus hernia are diagnosed initially with a suspicious image on a straight chest radiograph. On a straight chest radiograph, a diaphragmatic hiatus hernia presents as a faint mass behind the shadow of the heart. This fuzzy block can have water level - steam or not.
Figure B: image of a mediastinal air mass.
Source: A.H.A. Chapman, (2000)
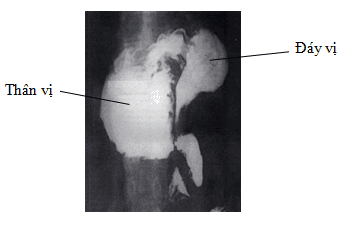
7.2. Contrast Esophageal - Gastric X-ray [1]: Contrast Esophageal - Gastric X-ray is one of the laboratory tests indicated to confirm the diagnosis of diaphragmatic hiatus hernia, providing information about the spread of the hernia mass, helping to distinguish sliding and rolling hernias to determine the location of the cardia.
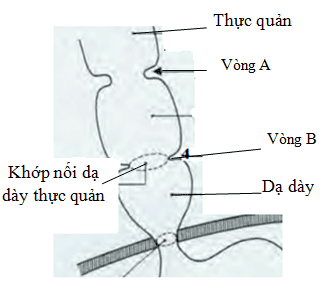
On a normal contrast-enhanced esophagogram, the B ring (gastro-oesophageal junction), may be located ≤2 cm above or below the esophageal opening.
In hiatal hernia, the hernia can be recognized in the presence of gastric mucosal folds inside the hernia sac. Torsion of the esophagus may have an eccentric articulation with the hernia mass.
Criteria for hiatal hernia type I: the hiatus is more than 3 cm wide, there are at least 5 mucosal folds running through the diaphragmatic fissure, the gastroesophageal junction moves higher than 2 cm above the diaphragm (normal). gastroesophageal junction is only ≤ 2cm).
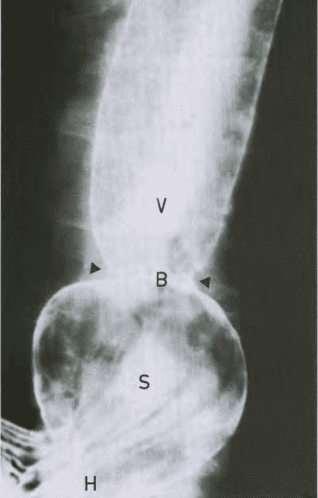
S: stomach above the diaphragmatic cleft
B: ring B (gastroesophageal junction)
V: esophagus
Source: A.H.A. Chapman, (2000)
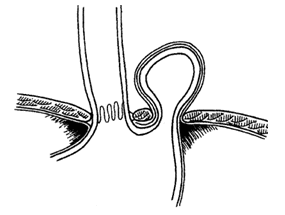
Schatzki ring:
Schatzki ring is a narrowing of the gastroesophageal junction, causing dysphagia, which may be congenital, or may be due to gastroesophageal reflux. Before dysphagia occurs, the lumen of the esophagus usually narrows to less than 13 mm. The ring of Schatzki is always associated with a small sliding diaphragmatic hiatus hernia, and is always evident when the esophagus is enlarged after taking Barium.
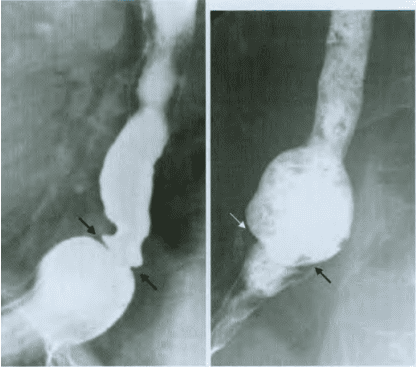
Figure B: bread soaked in Barium was swallowed and stuck at the Schatzki ring.
Source : A . H.A. Chapman, (2000)
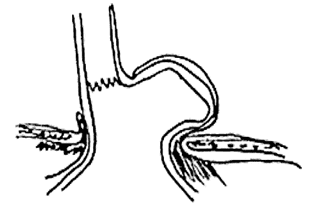
Type II diaphragmatic hiatus hernia:
Image of a contrast pouch located adjacent to the esophagus (differentiated from an esophageal diverticulum).
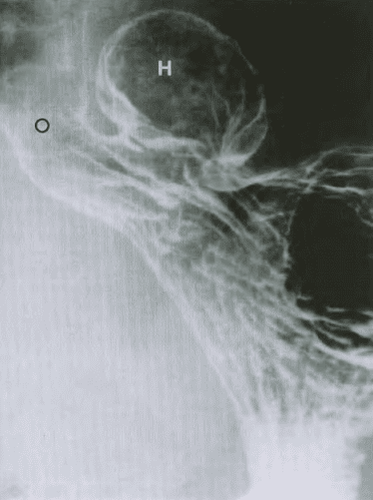
Type III hiatal hernia: the distal esophagus adjacent to the stomach is herniated and the gastro-oesophageal junction is located above the diaphragm.
Type IV hiatal hernia: in addition to the stomach, there are viscera such as colon, small intestine, large omentum in the hernia sac [1].

7.3 CT scan of thoracic and abdomen The image of esophageal hiatus hernia on CT scan is a mass (with or without air-water level) located behind the heart. The block can be traced to the diaphragm through subsequent slices. There are also signs such as: distance between the two diaphragms >15mm (normally ≤15mm), soft tissue dense mass protruding above the diaphragmatic fissure that may be surrounded by a large omentum.
CT scan provides valuable information on the location of the hernia mass and the organs involved (class IV). In particular, the 3-D reconstruction technique, which helps to evaluate the structure of the diaphragm column, its anatomical relation to the stomach, helps to guide the preoperative plan.
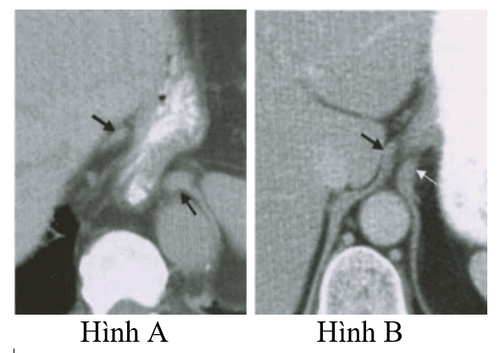
Figure B: CT scan image of the normal diaphragm: the distance between the two pillars very narrow.
Source: A.H.A. Chapman, (2000)
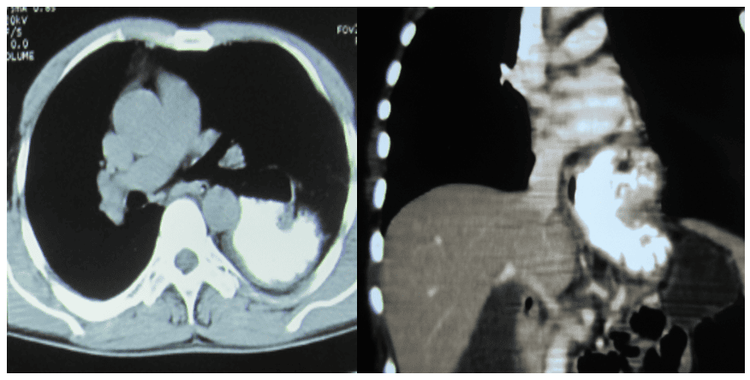
The esophagus is dilated, bell-shaped, with 2 rings: the proximal ring is formed by the lower esophageal sphincter, the distal ring is formed by the esophageal orifice. The length from the dental arch to the Z line is shortened: <35 cm. (normally this distance is 38 - 42 cm). The mucosal folds converge into the hernia opening. Machine retrograde position:
Heart is not tight with the mucosal folds converging to the hernia hole. Bell-shaped dilatation above the cardia. The ascent of the hernia during inspiration
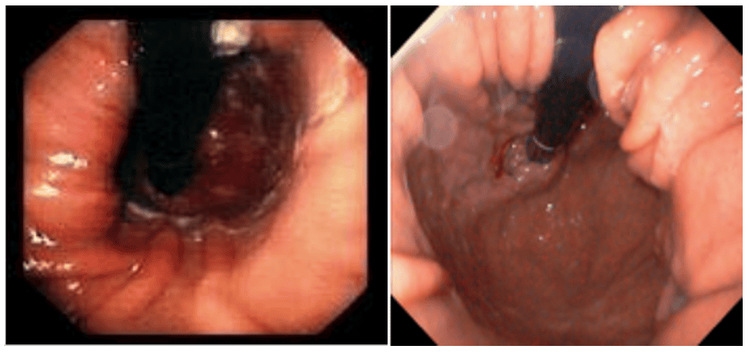
Type II: Only seen when the machine is inverted: the cardia is normal, there is another lumen next to the cardia, the mucosal folds converge into the hernia.
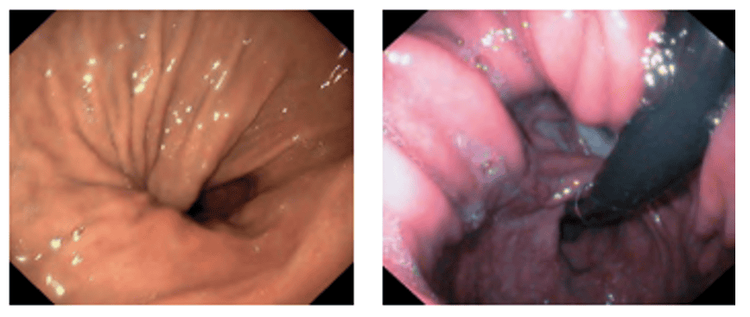
Type III: The image is a combination of the two images above, with the image of a hole next to the foramen, the cardia is not tight [12].
In addition to the definite diagnostic role, endoscopy is also useful in diagnosing complications of diaphragmatic hernia such as inflammation, ulceration, bleeding, or diseases related to the present. chronic reflux phenomena such as Barrett's esophagus, esophageal cancer.
7.5. Abdominal ultrasound In a normal person, the diameter of the alimentary canal (esophagus) at the esophageal slit is 7-10 mm. This size, when reaching 16 - 21 mm, indicates that it is not the esophagus but the stomach located in the esophageal hiatus. This sign has a positive predictive value of 100% and a negative predictive value of 90% in diagnosing diaphragmatic hernia.
7.6. Measurement of esophageal manometry and 24-hour esophageal pH [21], [44], [46], [53], [54], [60] Mainly used to evaluate reflux esophagitis, Esophageal dyskinesia, esophageal defects, or to rule out pathologies such as scleroderma, achalasia. A 24-hour esophageal pH measurement can also help evaluate reflux esophagitis in patients in whom esophagoscopy is normal.
8. Complications of diaphragmatic hernia
Complications of sliding diaphragmatic hernia:Reflux esophagitis, erosive esophagitis (Cameron's ulcer), esophageal ulcer. Bleeding from inflammatory lesions or ulcers of the esophagus. Blood is usually oozing, and massive bleeding is rare. Complications of a coiled hiatal hernia:
Approximately 30% of patients with a coiled hiatal hernia have ischemia, which can be caused by bleeding from the mucosa due to congestion of the vein at the foramen.
Approximately 30% of patients with slit diaphragmatic hernias have complications of reflux esophagitis. The greatest risk of a coiled hiatal hernia is gastric torsion, strangulation, leading to necrosis of the part of the stomach that is herniated.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for diaphragmatic hernias... Along with that, at the Hospital Vinmec, diagnostic endoscopy is performed through gastroscopy with Olympus CV 190 endoscope, with NBI function (Narrow Banding Imaging - endoscopy with narrow light frequency band) for image analysis results. mucosal pathology is more obvious than conventional endoscopy, detecting small herniated lesions. Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with gastroscopy and esophagoscopy services at Vinmec Hospital. Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.