This is an automatically translated article.
Diabetic skin disease is one of the common diabetes complications. The most common presentation is patches of hyperpigmentation or spots on the front of the legs. Skin lesions caused by diabetes are benign, which can disappear on their own after many years, especially when blood sugar is well controlled.
1. The concept of diabetic skin disease
Diabetes mellitus is a chronic disease with elevated blood glucose levels and insulin disturbances such as insulin deficiency and/or insulin resistance in peripheral tissues. Diabetes leads to metabolic disorders that damage many organs such as the heart, blood vessels, nerves, immune system, eyes and skin.
Diabetic skin disease is one of the common diabetes complications, causing the most common skin problems in people with diabetes. Diabetic skin disease is characterized by scaly, mildly concave skin lesions, often reddish or light brown, round or oval in shape and usually present on the front of the lower legs (found in 30% of patients with diabetes). Disconnect the road).
More than 50% of people with diabetes have skin problems. Although diabetic skin disease is common in people over 60 years of age, it can actually occur at any age, regardless of sex or race. The elderly, those with poorly controlled blood sugar or have the disease for 10 to 20 years are at high risk of diabetic skin disease.
2. Manifestations of diabetic skin disease
The most common manifestation of diabetic skin disease is patches or spots of hyperpigmentation on the front of the legs. Manifestations of diabetic skin disease include:
Patches of skin that are often flaky at first but then flatten and then slightly recede, known as atrophy. Skin patches range from pink to red or light brown to dark brown. Round or oval in shape. There may be multiple nodules covering a large area. Patches of skin lesions are rarely stinging, burning, open sores, or painful. In some of these patches of skin look like age spots. Diabetic skin disease usually appears mainly on the lower legs. Other less common sites include the scalp, forearms, the front of the thighs, the sides of the feet, and the trunk.

Hoại tử mô mỡ do tiểu đường là một trong tình trạng bệnh da do tiểu đường
3. Causes of diabetic skin disease
The exact cause of diabetic skin disease is unknown but may be related to diabetic nerve and vascular complications. One reason is that there are changes in the small blood vessels that lead to the leakage of cellular components from within the blood vessels into the skin.
Diabetic skin disease tends to occur in people who are older or have had diabetes for more than 10 years. In addition, skin disease is also significantly associated with increased glycosylated hemoglobin - a sign of poor glycemic control. Diabetic skin lesions often appear after trauma, thought to be an amplified tissue response to trauma.
4. Identify diabetic skin diseases
4.1 Diabetic foot Diabetes if not well controlled will lead to vascular damage and neurological complications. Diabetic foot with ulceration as a result of peripheral neuropathy (60-70%) or microvascular complications (15-20%) or a combination of the two causes circulatory failure complete and malnourished. Pressure sites, such as the feet, are prone to ulcers, which can lead to infection and gangrene. Diabetic foot occurs in about 15-25% of patients, of which 70% require amputation.4.2 Diabetic blisters Diabetic blisters are rare, acute lesions that occur commonly in patients with longstanding diabetes, severe disease, or multiple diabetic complications. , especially those with diabetic retinopathy and neurological complications .
Diabetic water bladder disease is more common in men than women, between the ages of 17 and 84 years old, with the following characteristics:
No itching, no pain, size from 0.5 to 17 cm Bubbles tense, no surrounding inflammatory halo Often appears on forearms, hands, fingers and lower legs, feet, toes, rarely trunk. Spontaneous blisters on the lower extremities can be the first sign of diabetes. Intra-epidermal blisters are sterile, fluid-filled blisters that usually heal on their own without scarring within 2–5 weeks. Subepidermal bullae are less common and may be hemorrhagic, which, when healed, usually results in scarring and atrophy of the skin. Diabetic blisters do not require treatment and most often heal on their own, it is important to avoid rubbing, not scratching or breaking the blister on your own, take care of cuts (if any) and avoid superinfection. .
4.3 Scleroderma Diabetic scleroderma is scleroderma-like skin changes that often occur in people with type 1 diabetes for many years. Scleroderma occurs in 10 to 50% of patients with diabetes, with an equal incidence in men and women. Pathogenesis is caused by products of increased glycosylation that thicken collagen. Manifestations of scleroderma is a condition where the skin is tight, thick like wax on the back of the hand, the fingers (usually at the proximal or intervertebral joints) become stiffer and difficult to move. Hard and swollen skin that may extend up to the forearm and forearm, bilaterally symmetrical, is painless. In some cases, the skin on the elbows, knees, or ankles also thickens and has an orange peel-like texture, making it difficult to flex the arms and legs. In addition, other sites can also be encountered are the shoulder, neck, upper back, chest and sometimes spread to the face.
Skin sclerosis occurs in patients with complications from diabetes or poorly controlled blood sugar. When thick, hard skin develops on the fingers, toes, and areas near or just above the joints, a useful treatment is physical therapy to help restore the ability to flex and extend the joints.

Hình ảnh xơ cứng da do biến chứng đái tháo đường
The pathogenesis of fat necrosis is unknown but may be due to inflammation of the small blood vessels in complications of diabetes. Fat necrosis manifests as atrophic epidermal patches, yellow-brown or red, wax-like, painless, and ulcerated on the surface. The margin of the lesion is red, raised, clearly demarcated. The skin around the necrotic area is smooth, shiny, with visible blood vessels, and may be itchy and painful. Most skin lesions appear on the lower legs (75% of cases are symmetrical), possibly on the feet, arms, scalp, or trunk.
4.5 Acquired leg pruritus Skin pruritus in the setting of diabetes can be due to many causes such as dry skin, yeast infection, neuropathy or peripheral vascular disease that causes poor circulation. Pruritus is the most common diabetic skin disease, occurring in 50% of young patients with insulin-dependent diabetes. The etiology of the disease is not clear, there may be involvement of microvascular disease, increased glycosylation, damage to the stratum corneum and accelerated skin aging.
4.6 Acanthosis nigricans is a very common skin condition in patients with insulin resistant diabetes. In addition, acanthosis nigricans also encounter a number of other endocrine diseases such as adrenal insufficiency, hypothyroidism. This condition is common in African-American, Portuguese, Hispanic and Southeast Asian populations with metabolic syndrome, particularly obesity. The pathogenesis of the disease is due to the increased insulin in the blood which activates the insulin growth factor-1 (IGF-1) receptor on the keratinocytes leading to the growth of the epidermis. Acanthosis nigricans manifests as thickened, dark, velvety smooth skin and hyperpigmentation, usually appearing in folds such as the neck, armpits, elbows, navel, groin, areola, and under the breasts.
4.7 Tumors with peduncles are benign, pink or brown, pedunculate tumors that often appear around folds such as eyelids, neck, armpits, and groin in the elderly, some cases appear in association with acanthosis nigricans. If multiple pedunctival nodules are present, it may be a sign of hyperinsulinemia or disturbances of carbohydrate metabolism in type 2 diabetes.
4.8 Yellow granulomatous granuloma may be the first sign. marker for untreated diabetes, with severe hypertriglyceridemia. Typical lesions are papules 1 - 4 mm in size, reddish yellow, on the extensor surfaces of the extremities and buttocks. Yellow granulomas often appear in waves and can aggregate into a large patch.
4.9 Scleroedema Scleroderma is a rare cutaneous manifestation of diabetes, usually occurring in patients with type 2 diabetes over 40 years of age and in males, rarely in female patients. Manifestations are hard, wood-like edema that cannot be pinched, decreased touch and pain sensations, diffuse and symmetrical skin lesions, may have erythema, mainly appear on the neck, shoulders and back , can spread to the face. The majority of patients develop scleroderma at the onset of insulin dependence, often with unsuccessful treatment and complications.
4.10 Kyrle's disease Kyrle's disease is a chronic inflammatory granuloma of the hair follicles, often affecting the extremities, trunk, scalp, and face. Lesions are pink, red, or hyperpigmented, highly pruritic, oyster shell-like in shape, thickened and centrally concave, clustered in a long streak (Koebner phenomenon). The cause of Kyrle's disease is unknown, but it may be due to an inflammatory skin reaction secondary to hyperuricemia, uric acid deposition, or scratches caused by scratching. Kyrle's disease is closely associated with 5 to 10% of patients with diabetes and chronic renal failure, often presenting as late as 10 to 30 years after diagnosis of diabetes and many months after dialysis.

Bệnh Kyrle là bệnh da do đái tháo đường
4.11 Dermatitis Erythema in diabetic patients occurs on the skin of the face, neck and extremities, possibly due to vasodilation.
4.12 Yellow-orange skin Yellow-orange skin lesions are well-defined, yellow-orange patches that appear above and around the eyelids, areas of skin with many sebaceous glands (face area), and areas with thick horny layers. (palms, soles). Fingernails and toenails can also have a similar yellow-orange tinge.
4.13 Follicular keratosis Folliculitis, resembling acquired ichthyosis, is a very common benign skin disease characterized by keratolytic papules around the hair follicles, mainly on the trunk. Lesions appear early in the course of diabetes.
4.14 Eruptive Xanthomas A yellow rash (Xanthomas) associated with elevated cholesterol and triglyceride levels in the blood. Presented by many tender and itchy, yellow or reddish-brown papules that suddenly break out all over the body, mainly on the backs of the hands, elbows, thighs, shins, feet, back of the knees, buttocks, and trunk; However, it can appear anywhere. Xanthomas most commonly occur in young, male, type 1 diabetic patients. Skin lesions appear suddenly and disappear quickly when the disease is well controlled.
4.15 Skin Infections (Bacterial, Fungal Infections) Skin infections can occur in 20-50% of patients with poorly controlled diabetes, mostly type 2 due to decreased blood circulation, decreased phagocytosis, and decreased phagocytosis. , impaired leukocyte adhesion and slow chemotaxis. Skin infections in people with diabetes can be caused by bacteria - including boils, ulcers, abscesses, cellulitis, or fungal infections, especially Candida albicans.
Fungal infections account for the largest proportion of diabetic skin infections, of which Candida is the most common. This is due to a weakened skin barrier. A fungal infection is also often the first warning sign of diabetes. Ringworm infections in patients with diabetes include: interstitial fungus, stomatitis, erysipelas, nail inflammation, vulvovaginitis, balanitis, cellulitis and, most seriously, infection. fungal sepsis. Patients with diabetic ketoacidosis are at increased risk of phycomycetes (mucormycosis) infections, especially in the oropharynx, with lesions in the form of central vascular necrosis, which can cause encephalitis. Most of these patients died. Bacterial skin infections are 3 times more common in patients with diabetes than in other diseases. Most infections are caused by gram-negative bacteria such as Pseudomonas aeruginosa. In addition, skin infections caused by poorly controlled diabetes include erysipelas, cellulitis, and pyoderma due to infection with gram-positive bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) or group A & B Streptococcus. In particular, infected diabetic foot ulcers is a symptom that should not be taken lightly because drug-resistant strains of Pseudomonas aeruginosa lead to severe sepsis, wound necrosis, and possibly amputation of the patient's limbs.
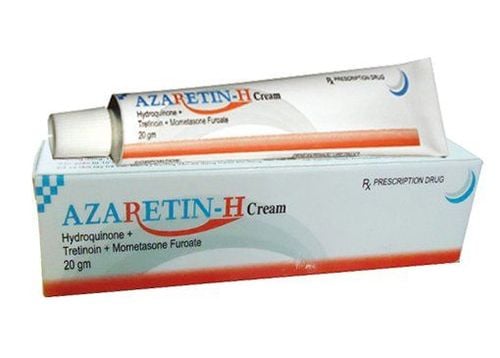
5. Treatment of diabetic skin disease
Skin lesions caused by diabetes are benign lesions that usually do not require specific treatment. With the exception of bacterial and fungal skin infections that require antibiotic and antifungal treatment, combined with daily wound care, remaining diabetic skin diseases tend to go away on their own after a few years. It may take a long time, especially when blood sugar is well controlled.
Therefore, the most effective measure to treat diabetic skin disease is to control blood sugar well by building a healthy diet with healthy foods, eating lots of green vegetables, fruits, whole grains, limit the intake of carbohydrates, animal fats instead use protein and oils from plants. At the same time, exercise regularly every day to maintain ideal weight and effectively improve insulin resistance. In addition, the damaged skin areas should also be kept moist, to avoid rubbing or trauma making the disease worse.
Vinmec International General Hospital is a prestigious address for examination and treatment with a sterile operating room system to avoid hospital infections. If you have a need for medical examination with experienced doctors at Vinmec, please make an appointment on the website to be served.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.