This is an automatically translated article.
Diabetic neuropathy is damage to the nerves that occurs as a result of diabetes, it can affect different parts of the body, and symptoms can range from mild to severe; The most common complication of diabetes1. What is diabetic neuropathy?
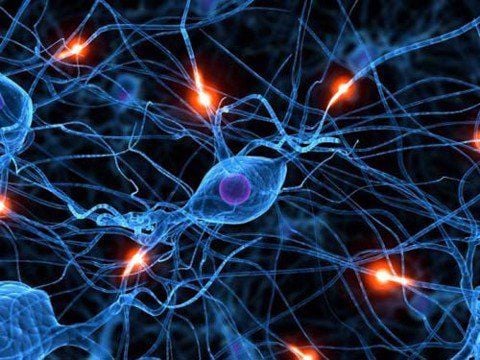
Diabetic neuropathy is a complication of diabetes that leads to damage to the nervous system. This is a progressive disease and symptoms get worse over time. Neuropathy occurs when high levels of fat or sugar in the blood damage nerves in the body. It can affect almost any nerve in the body, with a wide range of symptoms.Nerves are essential for the way the body works. They allow people to move, send messages about how things are feeling, and control automatic functions, such as breathing.
Some involve peripheral nerves, while others damage the nerves that supply internal organs, such as the heart, bladder, and intestines. In this way, it can affect many bodily functions.
2. Types of nerves
Four main types of neuropathy can affect the nervous system, including:Peripheral symmetric neuropathy: This affects the feet and hands. This is the most common form of diabetic neuropathy. Autonomic neuropathy: This occurs in the nerves that control involuntary body functions, such as digestion, urination, or heartbeat. Thoracic and lumbar radiculopathy, or proximal neuropathy: This damages nerves along a specific distribution in the body, such as the chest wall or legs. Mononeuropathies: These diseases can affect any nerve. The symptoms of neuropathy depend on the type and the nerves involved.
3. Signs and symptoms
Signs and symptoms of diabetic neuropathy usually take several years to appear. Signs and symptoms will depend on the type of neuropathy and the nerves it affects.3.1 Peripheral Neuropathy Symptoms of Peripheral Neuropathy include:
Numbness, pain, tingling and burning sensation that begins in the toes and fingers then continues up the legs or arms Loss of tone muscle force in the hands and feet Unable to feel heat, cold, or physical injury loss of balance Charcot joint, in which the joint is damaged by nerve problems, often in the feet Peripheral neuropathy affects to the feet can make it difficult for a person to stand and walk. It can increase your risk of falling. When a person cannot feel heat, cold or is injured, this can lead to new problems. For example, a blister on the foot may become ulcerated because the patient does not feel pain in the early stages. As the infection progresses, gangrene may develop. Eventually, amputation may be necessary.
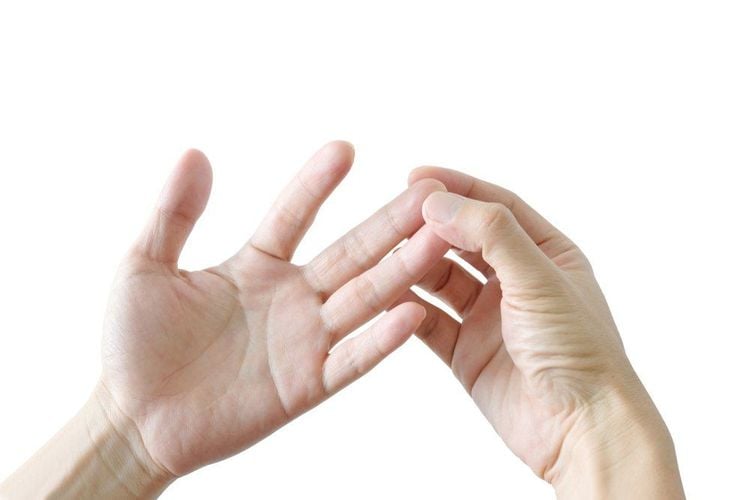
Cảm giác tê, đau ở đầu ngón tay, ngón chân là triệu chứng bệnh thần kinh ngoại biên ở người tiểu đường
acidity and bloating Nausea, constipation, or diarrhea Unrecognized hypoglycemia, in which a person does not feel the effects of intake low sugar Difficulty speaking or swallowing Feeling full after eating small amounts of food Vomiting several hours after eating Orthostatic hypotension, or feeling light-headed and dizzy when standing up Faster-than-normal heartbeat Sweating excessive sweating, even in cool temperatures or at rest Bladder problems, for example, difficulty emptying the bladder completely when urinating, leading to urinary incontinence Male sexual dysfunction and female Sensory disturbances or distorted sensations Significant eyelid drooping on the face and eyelids Muscle spasms and weakness. 3.3 Other Types There are many types of neuropathy. Proximal neuropathy can lead to pain in the lower body, often on one side, and weakness in the legs.
Symptoms of focal neuropathy can vary widely, depending on the nerve affected. Focal neuropathy and cranial neuropathy can both lead to visual disturbances, such as diplopia.
People with diabetic neuropathy often don't realize they have it until symptoms are more advanced.
4. Diagnosing Diabetic Neuropathy
Your doctor will do a physical exam and examine your feet to check for:Ankle reflex Loss of sensation Changes in skin texture Changes in skin color Other tests may include: Checking for blood pressure and rhythm fluctuations heart. If your doctor suspects diabetic neuropathy, they may run some diagnostic tests, such as:
An electromyogram (EMG), which records electrical activity in the muscles A speed test Nerve conduction (NCV) records the rate at which touch signals travel through nerves.
5. Treatment of diabetic neuropathy
Most types of diabetic neuropathy get worse over time. The first step for people with any kind of illness is to bring their blood sugar into the doctor-approved target range and control high blood pressure and cholesterol levels.Management of glucose levels will minimize the risk of diabetic neuropathy. An important part of treatment focuses on reducing pain and controlling some symptoms.
Certain medications and types of physical therapy can help control the pain of diabetic neuropathy, along with other treatments. However, they cannot repair the nerves.
People should also avoid or stop smoking and limit alcohol intake to a maximum of one drink per day for women and two drinks for men.
5.1 Medication Use Medications that can help control pain include:
Anticonvulsants Opioid tricyclic antidepressants and non-Opioid pain relievers Opioid use can lead to dependence, so doctors should be prescribed in as low a dose as possible. A person with diabetic neuropathy may use other types of antidepressants, such as Serotonin-Norepinephrine inhibitors, to target other painful symptoms of diabetic neuropathy.
Lotions, creams, and some supplements, such as topical ALA or capsaicin, can also help with pain.

Bác sĩ có thể kê các loại thuốc để kiểm soát cơn đau đối với bệnh thần kinh đái tháo đường
Electrical nerve stimulation is a painless type of physical therapy that can help reduce stiffness and promote healing of foot ulcers.
Gadget training includes a reassessment of how to walk. It helps prevent and stabilize foot complications, such as ulcers and injuries. This type of physical re-education is important for people using prostheses after a limb loss if diabetic neuropathy leads to amputation.
A good physical therapist will ensure that exercises for people with diabetic neuropathy don't injure the feet, which can be sensitive.
Other therapies include devices that a person can use to keep painful or sensitive limbs from touching a bed or chair.
Chiropractors, massage therapists, or chiropractors can perform regular massage or manual therapy to stretch muscles. Massage can inhibit contractions, spasms and muscle atrophy caused by poor blood supply.
Specific exercises, such as swimming or aerobics, can help an individual develop and maintain muscle strength and reduce the loss of muscle mass.
Ultrasound therapy is another type of physical therapy that uses very high frequency sound waves to stimulate the tissues beneath the skin. This can help some people regain sensitivity in their feet.
6. Complications occur
Diabetic neuropathy can contribute to a number of high-risk complications, from changes in heart rhythm to visual disturbances. Possible complications include loss of sensation in the feet.This can lead to not being able to feel cuts or sores, and infection as a result. If left untreated, infection in the limb can lead to amputation.
Serious bladder and kidney infections can also occur, causing health problems. To prevent complications of diabetic peripheral neuropathy, good foot care is essential.
People with this condition should check their feet every day for sores or sores.
Smoking also increases the risk of foot diseases in people with certain types of diabetic neuropathy. A podiatrist can help with foot care, and a health care provider can offer advice about quitting smoking.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.