This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Data on Helicobacter pylori (H. pylori), has accumulated over 40 years since its description as a etiological factor in gastrointestinal diseases. The majority of modern publications are devoted to the study of the pathogenic properties of microorganisms in the development of chronic gastritis, peptic ulcer disease and gastric cancer, as well as the methods of eradicate it.
However, in recent years, more and more studies have suggested that H. pylori has beneficial or potentially positive effects on the human body. The authors attempted to objectively analyze the information accumulated in the literature on H. pylori.
1. Some studies suggest that H.pylori may be part of the composition of the human microbiome
Some studies consider it to be one of the recently identified human bacterial pathogens and pay particular attention to evidence suggesting that it may be part of the composition of the microbiome. in humans as a commensal (from French to English commensal) or even as a symbiotic. The data presented discussing the presence or absence of an effect of H. pylori on human health suggest that there is a clear ambiguity of the matter. A re-evaluation of the available data on H. pylori infection is important to answer the question of whether there is a need to establish a program for mass eradication of H. pylori or adopt a more personalized approach to management. treatment of patients with H. pylori-related gastrointestinal diseases and to implement eradication therapy.
2. Development of rare symptoms with high prevalence in the population
After the discovery of R. Warren and BJ Marshall, the concept of pathogenesis and treatment regimens for peptic ulcer disease mainly involves the identification and eradication of H. pylori. It is now known that the prevalence of H. pylori is high in healthy individuals (about 50% of the population worldwide and more than 70% in developing countries). H.pylori infection is usually acquired during childhood and usually persists for life. Thus H.pylori infects the majority of the world's population for most of their lives and in most cases causes no symptoms. The course of infection in H. pylori is chronic and only one in ten colonize; The most common is the elderly, clinical manifestations many years later.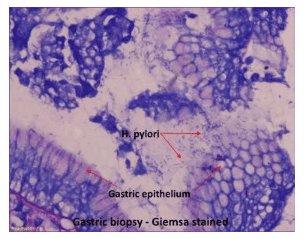
Only 5%-10% of people infected develop symptoms of gastritis or peptic ulcer disease
Tsimmerman reports that less than 1% of people infected with H. pylori develop various diseases and about 70% of people found to have the bacteria are carriers of the good bacteria. Available data show that only 5%-10% of those infected develop symptoms of gastritis or peptic ulcer disease. Furthermore, the review data (Araújo et al.) indicate that the detection rate of H. pylori infection in patients diagnosed with peptic ulcer disease does not differ from the prevalence of H. pylori infection in the general population. Generally speaking. The authors also note that in 20%-50% of cases of peptic ulcer disease, they were unable to identify an overarching etiology of the ulcerative lesion, that is, an idiopathic ulcer. (Gastroenteritis/NSAIDs/NSAIDs are negative for H. pylori). Sidorenko stated that the presented data provide a strong argument against the leading role of H. pylori in the development of gastrointestinal diseases. The wide spread of H. pylori infection among people with no clinical signs and the low incidence during chronic colonization of the gastric mucosa clearly suggest that H. pylori is more likely to be an opportunistic or latent pathogen rather than an actual pathogenic bacterium. The data presented suggest that the infectious theory of chronic gastritis, peptic ulcer disease and gastric cancer seems to be an exception to the rule. In addition, the severity of chronic gastritis and/or peptic ulcer disease appears to be directly related to other etiological factors, along with the density of H. pylori infection.
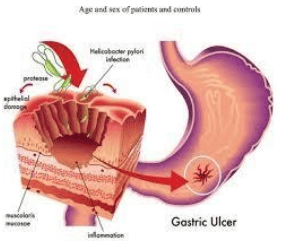
3. H. pylori and peptic ulcer disease
Peptic ulcer disease is a chronic multifactorial disease characterized by an imbalance between the active components of the gastroduodenal contents and the protective mechanisms of the gastric mucosa. An important role in the pathophysiological changes characteristic of peptic ulcer disease is played by important components, such as genetic predisposition, psychosocial and psychosocial stressors, autonomic dysfunction, local pathogenesis (acidity of the stomach), immunodeficiency states, oxidative stress, smoking, excessive alcohol intake, and use of steroids and non-steroidal anti-inflammatory drugs steroids. In their review, Malfertheiner et al focused on the fact that the development of peptic ulcer disease depends on complex influences and/or a combination of both exogenous and endogenous factors.
The most important endogenous components of ulceration
In addition to the exogenous factors described above, the most important endogenous components of ulceration are the extent and complete function of the ulcers. intestinal hormones (gastrin, somatostatin), genetic predisposition factors (parietal cell count, basal level of gastric secretion of hydrochloric acid, and defect in bicarbonate secretion). Such observations suggest that the presence of H. pylori infection may be a single (but very brief) component in the etiology of ulcerative disorders. It is essential to also recall the fact that in cases where Helicobacter is the cause, the risk of developing this disease depends on the genotype of the H. pylori bacteria: The patient has a confirmed diagnosis of the disease. peptic ulcers were found to be Vaca-positive and cagA-positive genotypes. At the same time, genotypes containing the vacA gene are known to account for approximately 60% of all detected Helicobacter forms. In addition to H. pylori ulcers, the current classification also identifies tumor ulcers, ulcerative lesions in Zollinger-Ellison syndrome, Crohn's disease, eosinophilic gastroenteritis, and lesions. radiation and viral infections (cytomegalovirus or herpes virus infection in immunocompromised patients). The idiopathic form occupies a place of its own.
Epidemiological studies in recent years show an increase in progression of idiopathic forms of peptic ulcer disease with a decrease in the global prevalence of H. pylori infection. Interestingly, epidemiological studies Epidemiological studies in recent years have shown an increase in progression of idiopathic forms of peptic ulcer disease with a decrease in the global prevalence of H. pylori infection. Thus, Indian researchers showed that 45.9% of peptic ulcer and 29.6% duodenal ulcer cases were idiopathic (they were not related to H. pylori detection or history of steroid intake. / NSAID). Reshetnyak et al. presented data on the role of H. pylori and drugs in the development of gastric mucosal lesions (GM) in patients with systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS) ). Endoscopy of patients with SLE and APS revealed the following GM changes: gastroenteritis (82.4%), cachexia (24.7%), hemorrhage (8.2%), and epigastric inflammation (8.2%) ,2%). The prevalence of H. pylori infection in patients with SLE and APS was similar to that in the general population. The authors' data showed no direct correlation between the observed GM changes and H. pylori infection. However, treatment with glucocorticoids, low-dose acetylsalicylic acid, NSAIDs, and anticoagulants in this case was responsible for GM lesions in SLE and APS patients. There is evidence that the most favorable course of ulcers is associated with H. pylori compared with other diagnosed types.
Kanno et al determined that out of 382 examinees, a diagnosis of peptic ulcer disease was found. , patients with confirmed diagnosis of H. pylori-positive ulcer had a statistically significant increase in healing rate. In the study, the patients were divided into 4 groups: Group due to H. pylori alone; an H. pylori(+) / NSAID group (+); a group of simple NSAIDs; and the idiopathic ulcer group (IPU). Indices, such as 3-month cure rate, course of treatment and relapse rate, were estimated. According to the data presented, cure rates in these groups were distributed as follows: 95.0%, 94.9%, 73.3% and 77.4%, respectively. This index for different idiopathic forms is statistically significant (P < 0.01). The recurrence rate in the idiopathic ulcer group was also much higher: 13.9% in the idiopathic ulcer group and 2.1% in the H. pylori group alone (P < 0.01). The cumulative recurrence rate estimated by the Kaplan-Meier method in the idiopathic ulcer group was also significantly higher in the idiopathic ulcer group than in the simple H. pylori group (P = 0.015). Rasane et al. demonstrated that patients with peptic ulcer disease without H.Pylori had a more severe disease course and a more negative prognosis than those with H. pylori-associated disease. Therefore, the albumin level in the H.Pylori-free group was higher than in the H. pylori-positive group: 2.97-0.96 compared with 3.86-0.91, P = 0.0001. The same pattern was observed when assessing the patient's condition on admission: In the H.Pylori-free group, scores on scales, such as the American Society of Anesthesiologists' scoring system, were observed. and Charlson comorbidities index, much higher: 3.11-0.85 compared with 2.60-0.73 (P = 0.005) and 4.81-2.74 compared with 2.98-2.71 ( P = 0.004), respectively. There are also significant differences in indicators, such as length of hospital stay: 20.20-13.82 versus 8.48-7.24; P = 0.0001 and 30-day read rate (11; 29.73% vs 5; 11.91%; P = 0.049). The variety of causes that lead to the ulcer process allows peptic ulcer disease to be considered a polygenic and polygenic disease
When H. pylori was discovered, there were many theories about the development of the disease. Peptic ulcer: Hypotheses on vasculitis, gastritis, allergy, hormonal, motor, corticovisceral, neurological, psychiatric, and acidosis theories. Each of them deserves attention, as it reflects one of the facets of this complex issue. The above data suggest that for people with a predisposition to this pathology, the emergence of the infectious theory has become an important and significant addition to the already existing etiological factors. In addition, not in all cases, but only in a certain state of microorganisms, H. pylori becomes a pathogen and an additional cause of chronic gastritis, peptic ulcer disease, and even stomach cancer.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Reshetnyak VI, Burmistrov AI, Maev IV. Helicobacter pylori : Commensal, symbiont or pathogen? . World J Gastroenterol 2021; 27(7): 545-560 [PMID: 33642828 DOI: 10.3748/wjg.v27.i7.545]