This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
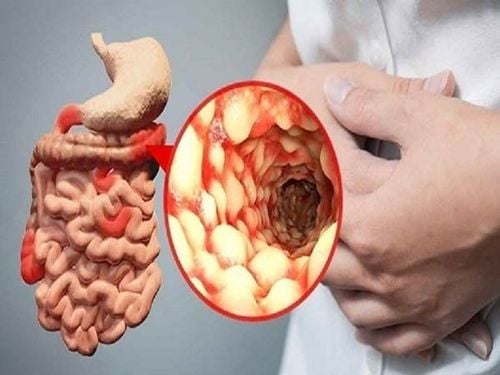
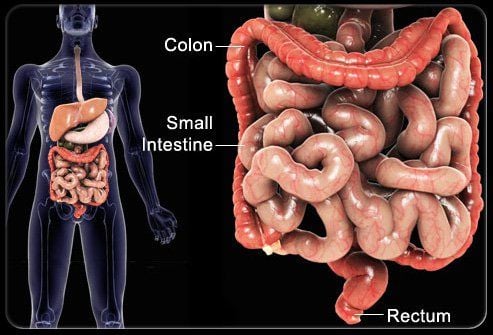
Gastrointestinal complications in kidney transplant recipients can result from infections that are typical of organ transplant recipients, such as post-transplant cytomegalovirus (CMV) colitis, and kidney damage. Immunosuppressive-mediated injury to the gastrointestinal mucosa. Immunosuppressive therapy, which could theoretically combat this inflammatory process, could conversely allow dysregulation of the intestinal immune system, ultimately leading to the development of post-transplant IBD.
1. Cytomegalovirus (CMV) Colitis
Infectious complications are the most important cause of morbidity and mortality after transplantation. Incidence varies with many factors, including the type of transplant, the patient's immune system, and immunosuppressive therapy. It is estimated that about 80% of organ transplant recipients experience post-transplant infection, and the gradual decline in the acute rejection rate has led to a significant increase in infectious diseases, especially those associated with latent viruses such as CMV. Although the application of CMV prophylaxis has significantly reduced the incidence of clinically manifest CMV disease in the early post-transplant period, CMV is the virus most commonly infecting patients undergoing treatment. solid organ transplantation, with significant consequences for graft and patient survival. During the first year after transplantation, 50%-70% of patients develop primary infection, reactivation, or reinfection.
2. Pathogenesis
When CMV infection causes significant viral replication and causes symptomatic disease, it can cause tissue-invasive disease with viral end-organ damage. The gastrointestinal tract is most commonly affected during CMV tissue invasive disease, resulting in esophagitis, gastritis, enteritis, or colitis. Diagnosis requires biopsies obtained during esophagoscopy and/or colonoscopy with histological or culture-based evidence of CMV. Gastrointestinal involvement during CMV infection has been described in approximately 5% of patients undergoing solid organ transplantation and may involve any part of the gastrointestinal tract, but incidence may increased to 25% in patients with clinical symptoms suggestive of CMV infection.
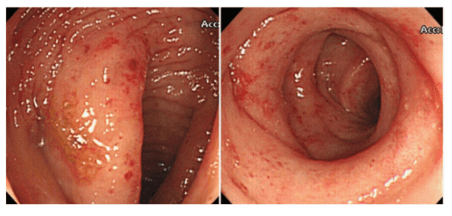
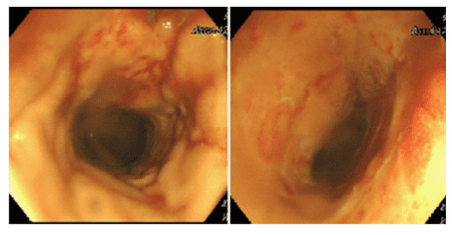
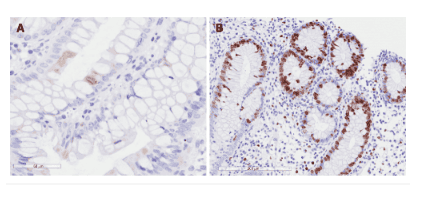
3. Endoscopic signs and histopathology
Endoscopy has a variety of lesions ranging from patchy congestion, exudative and erosive inflammation to oozing mucosa with numerous erosions. The main histological feature of CMV colitis is increased apoptosis of enterocytes, which is caused by viral infection, so it is difficult to distinguish CMV colitis from GVHD (graft-host disease) on gastrointestinal biopsy. Definitive diagnosis in renal transplant patients requires histological findings of characteristic reservoirs on haematoxylin and eosin staining (Figure 3), in addition to gross lesions on endoscopic examination. Furthermore, the detection of CMV in formalin-fixed tissue by immunohistochemistry, which is ultimately integrated with polymerase chain reaction (PCR) of paraffin-embedded tissue, is a highly valuable method for confirming the diagnosis of inflammation. colon due to CMV.
4. Serological test
Serological testing (for CMVIgG) is not effective for the diagnosis of CMV disease because most cases present in latent viral reactivation. The late CMV antigen PCR assays and the quantitative CMV PCR assay are highly sensitive for CMV virus, but they are not good predictors of CMV tissue invasive disease and have poor sensitivity (range, 48). %–73% ) in the detection of gastrointestinal disease. In a recent study, Durand et al evaluated the sensitivity of quantitative PCR (qPCR) for CMV deoxyribonucleic acid in plasma for the diagnosis of gastrointestinal CMV infection. Of the 81 solid organ transplant recipients (liver and kidney), 20 cases of GI CMV that were demonstrated by endoscopic biopsy were identified. Overall, the sensitivity of qPCR for the diagnosis of CMV gastrointestinal disease is 85% and specificity is 95%. Interestingly, the sensitivity of qPCR in CMV seronegative recipients to CMV seropositive (D+/R-) recipients was 100%, while in CMV D+/R+ recipients it was 72 .3%, possibly due to differences in immune responses. Indeed, in patients with CMV R, gastrointestinal CMV disease is a consequence of primary acute viremia. In contrast, in CMV R+ patients, gastrointestinal disease occurring following CMV reactivation may be limited by pre-existing immunity.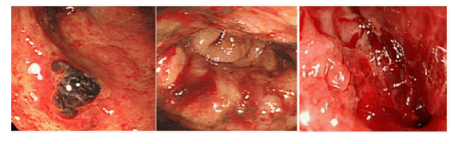
5. Treatment of CMV colitis after kidney transplant
Treatment of CMV colitis involves reducing immunosuppression and administering specific endothelial antiviral drugs, such as IV ganciclovir (5 mg/kg BID) for a period of 10-14 days until upon resolution of symptoms, followed by oral valganciclovir (900 mg once daily) for 3-6 months. High-dose valganciclovir (up to 1800 mg twice daily) and/or foscarnet and cidofovir with reduced immunosuppression may be a treatment option for ganciclovir-resistant CMV colitis.
Conclusion
Gastrointestinal diseases are common after kidney transplantation and can present with a variety of clinical and histological features. The diagnosis and management of post-transplant IBD is challenging because there are no definite histological criteria to unambiguously diagnose post-transplant IBD. Indeed, many histological features may be common among different clinical forms, such as mycophenolate mofetil colitis with Graft-host disease, and this can be controversial in its management. The management of post-transplant IBD can be challenging due to the current use of immunosuppressive therapy, which may increase the risk of infectious complications. Furthermore, the clinical course of post-transplant IBD may be more severe than that of IBD in the general population. A better definition of clinical and histological features may help standardize treatment and improve the outcome of IBD after transplantation. Due to the clinical complexity of the IBD patient.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Gioco R, Corona D, Ekser B, Puzzo L, Inserra G, Pinto F, Schipa C, Privitera F, Veroux P, Veroux M. Gastrointestinal complications after kidney transplantation. World J Gastroenterol 2020; 26(38): 5797-5811 [PMID: 33132635 DOI: 10.3748/wjg.v26.i38.5797]