This is an automatically translated article.
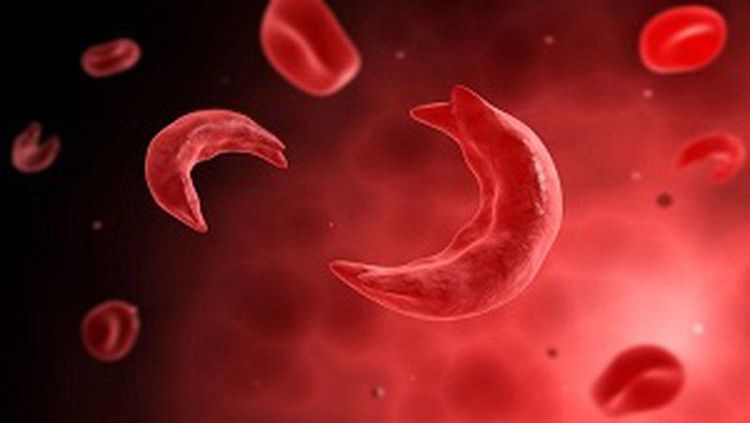
The article was written by Dr. Ngo Anh Tien – Vinmec tissue bankSickle cell disease (SCD) is a group of genetic disorders that affect hemoglobin, a molecule in red blood cells that carries oxygen around the body. People with this disorder have atypical hemoglobin molecules called hemoglobin S, which can distort red blood cells into a sickle, or crescent shape.
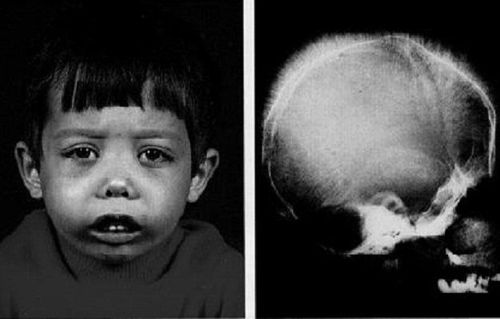
1. Sickle cell disease usually presents early in life
In the sickle-shaped form, red blood cells are easily broken, resulting in low red blood cells causing anemia, jaundice, shortness of breath, fatigue and growth retardation. Under vascular pressure, sickle cells easily stick together, causing blockage of small blood vessels. Patients will experience pain due to organ damage, especially in the lungs, kidneys, spleen and brain.
Pulmonary hypertension is caused by increased blood pressure in the blood vessels supplying the lungs. Statistically, about a third of adults have sickle cell disease and can lead to heart failure. This disease can be easily diagnosed, but treatment is a big challenge. This is an inherited genetic disorder, so the only effective treatment known to medicine today is stem cell therapy.
Accordingly, hematopoietic stem cells will be cross-transplanted into the patient's body. When these cells are received by the body, new, healthy blood cells are produced. The challenge is, how to ensure that the patient's immune system will not reject the transplanted foreign cells into the body?
A recent study published in the journal Bone Marrow Transplantation has shown breakthrough and very promising signals in the treatment of sickle cell disease based on the role of human leukocyte antigen compatibility ( Human Leukocyte Antigen (HLA) in hematopoietic stem cell transplantation from unrelated donors.
Ở dạng hình liềm, hồng cầu dễ bị phá vỡ, dẫn đến hồng cầu thấp khiến trẻ bị thiếu máu
In recent years, along with the development of regenerative medicine, cord blood has become a particularly important donor because of many advantages:
Contains an abundant source of primitive hematopoietic stem cells; Easy to take (doesn't cause any pain or harm to the recipient); Long term storage; Can be used repeatedly with stem cell proliferation technology; Customers can refer to:
Goodbye to the worry about the volume of cord blood
FDA (US Food and Drug Administration) has approved the treatment using cord blood of siblings effective equivalent to the use of bone marrow.
Especially for families with a history of blood diseases, it is advisable to store cord blood for the babies. Because sickle cell disease is a recessive genetic disorder, it may not manifest in one person, but will in the other.

Lưu trữ tế bào máu cuống rốn có thể được sử dụng hiến tặng cho cộng đồng, mang lại cơ hội cứu trị cho các bệnh nhân khác
At that time, umbilical cord blood will be the survival hope of the sick person. If fortunately none of the children show signs of the disease, cord blood can be used to donate to the community, providing a chance for other patients to be cured. But not all patients achieve this condition. Either because there are no siblings, or because the parents do not have access to cord blood storage information.
Therefore, the scientists conducted a review of the treatment outcomes for patients with SCD who received a heterozygous hematopoietic stem cell transplant, focusing on HLA compatibility.
The research team looked at data from 71 people with SCD who had been treated with a hematopoietic stem cell transplant at one of 23 European blood and marrow transplant centers between 2005 and 2017.
Mean age of group at the time of treatment was 9.3 years (2 to 47 years old), with 87% of cases aged 16 years or younger. In which, there are 31 recipient-donor pairs with HLA compatibility reaching 10/10, 20 pairs reaching 9/10 and 4 pairs reaching 8/10. The remaining 16 pairs did not have specific HLA data. The scientists divided into two groups the comparisons between pairs that were fully HLA compatible, and pairs that were less compatible. The data showed that after 3 years of transplantation, the survival rate of the first group was 96%, compared with 75% for the other group.
Besides, the elimination rate of the first group is also lower, about 31% compared to the 50% rate of the other group. Proving HLA compatibility between patients and non-blood donors is a very important factor affecting transplant results.
Thus, it can be concluded that finding a donor that is compatible with HLA 10/10 will bring a higher chance of survival and a lower rejection rate for the patient. But it should be noted that, only 31/71 transplants achieve this rate, and finding a donor has been a difficult journey.
Therefore, cord blood remains the safest, economic option for families. Stock up on this precious bioinsurance, not only for yourself but possibly, it also gives hope to society.
Đội ngũ cán bộ nhân viên thuộc Ngân hàng mô Vinmec
Currently, Vinmec Tissue Bank is the leading address in Vietnam with modern and advanced facilities meeting international standards. The bank is also under Vinmec Company, which holds many of the latest technologies in stem cell application in the treatment of a number of incurable diseases. Vinmec tissue bank is offering cord blood stem cells, cord stem cells, adipose tissue stem cells, and bone marrow stem cells.
Customers wishing to use the service should contact Vinmec Tissue Bank via:
Hotline: 0936 246 199
Email: v.biobank@vinmec.com
Directly contact Vinmec International General Hospital, 458 Minh Khai, Hai Ba Trung District, Hanoi.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to sources: parentsguidecordblood.org, ghr.nlm.nih.gov, sicklecellanemianews.com