This is an automatically translated article.
The article was professionally consulted with Specialist Doctor I Phan Dinh Thuy Tien - General Internal Medicine - Department of Medical Examination & Internal Medicine - Vinmec Nha Trang International General Hospital.The conduction system in your heart is the network of nodes, cells, and signals that control your heartbeat. Each time your heart beats, electrical signals travel through your heart. These signals cause different parts of the heart to relax and contract. Dilation and contraction control blood flow through your heart and body.
1. What is the conduction system in the heart?
The heart's conduction system consists of cardiac muscle cells and conductive fibers (not nerve tissue) that are used to initiate impulses and conduct them rapidly through the heart. They initiate the normal cardiac cycle and coordinate the contraction of the chambers of the heart. Both atria contract together, as do the ventricles, but atrial contraction occurs first.Your heart is a pump that carries blood around your body. For each heartbeat, electrical signals travel through conduction pathways in the heart. It begins when your sinoatrial (SA) node produces an excitatory signal.
1.1. Sinus atrial node
The sinoatrial (SA) node is an axial structure composed of a fibrous tissue matrix with closely arranged cells. It is 10-20 mm long, 2-3 mm wide and thick, with a tendency to narrow toward the inferior vena cava (IVC). The SA node is located less than 1mm from the epicardial surface, lateral to the right atrium at the anterior junction of the superior vena cava (SVC) and the right atrium (RA)(1)Arteries supplying The sinus node branches from the right coronary artery in 55-60% of hearts or the left circumflex artery in 40-45% of hearts. The artery approaches the node clockwise or counterclockwise around the junction between the superior vena cava and the right atrium.(1)
Internally dense sinoatrial node with adrenergic nerve terminals and postganglionic cholinergic. Neurotransmitters regulate the discharge rate of the sinoatrial node by stimulating beta-adrenergic and muscarinic receptors. Both beta 1 and beta 2 adrenoceptor receptor subtypes are present in the sinoatrial node. The human sinoatrial node contains three times greater density of beta-adrenergic and muscarinic cholinergic receptors than adjacent atrial tissue.(1)
1.2. Intra-atrial conduction
Anatomical evidence suggests the presence of 3 conduction pathways in the atria:Anterior internodal tract Median internodal tract Posterior internodal pathway. The anterior internode line begins at the anterior edge of the sinoatrial node and curves forward around the superior vena cava to enter the anterior interventricular band, known as the Bachmann bundle. This band continues to the left atrium (LA), with the anterior insular tract entering the superior border of the atrioventricular node. The bundle of Bachmann is a large muscle that appears to conduct cardiac impulses preferentially from the right atrium to the left atrium.
The median interventricular line begins at the superior and posterior margins of the sinus node, travels posteriorly to the superior vena cava to the apex of the atrial septum, and descends within the atrial septum to the superior edge of the AV node.(1)
The posterior interventricular line begins at the posterior edge of the sinus node and passes posteriorly around the superior vena cava and along the terminal part of the crestal crest to the apex of the eustachian valve and then enters the interatrial septum above the coronary sinus. , where it joins the posterior portion of the atrioventricular node. These groups of internodal tissue are best referred to as internodal atrial myocardium, not tubules, as they do not appear to be histologically discrete specialized tubes.(1)
1.3. Atrioventricular node
The compact portion of the atrioventricular (AV) node is a superficial structure located just below the right atrial endocardium, anterior to the coronary sinus opening, and just above the insertion of the tricuspid septal leaflet. It is located at the apex of a triangle formed by the tricuspid annulus and ligament of Todaro, originates in the central fibrous body and passes posteriorly through the atrial septum to continue with the Eustachian valve.In 85-90% of the human heart, the artery supplying the atrioventricular node is a branch from the right coronary artery that originates at the posterior intersection of the atrioventricular groove and the interventricular groove (Crux). In the remaining 10-15% of hearts, a branch of the circumflex coronary artery supplies the atrioventricular nodal artery. The fibers in the inferior part of the atrioventricular node may exhibit automatic impulse formation. The main function of the atrioventricular node is to regulate the transmission of impulses from the atria to the ventricles to coordinate atrial and ventricular contractions.
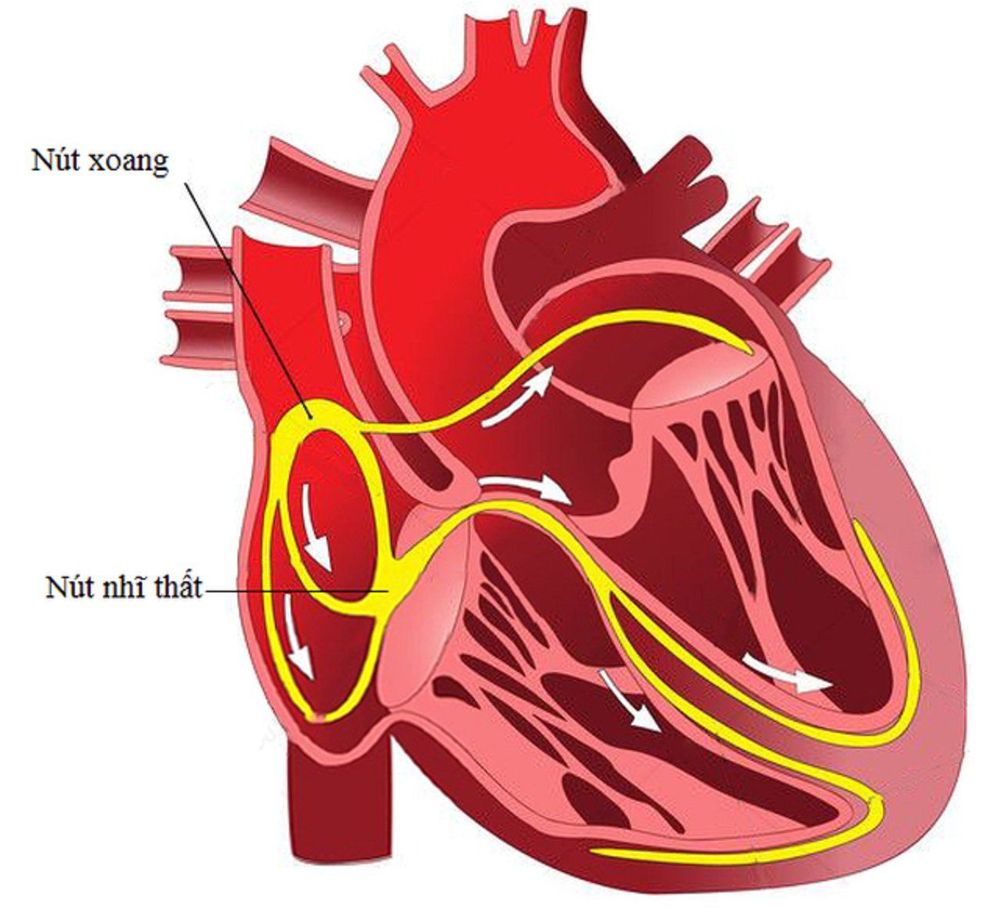
Hệ thống dẫn truyền trong tim bao gồm các tế bào cơ tim và các sợi dẫn
1.4. The bundle of His carries signals to the Purkinje fibers
The bundle of His is a structure that connects to the distal portion of the atrioventricular nodal block that passes through the central fibrillar body and continues through the annulus fibers, where it is termed the unbranched portion as it penetrates the membranous septum. The connective tissue of the central fiber body and the membranous septum enclose the penetrating part of the atrioventricular bundle, which can introduce extensions into the central fiber body. The proximal cells of the infiltrates are heterogeneous and resemble those of the atrioventricular nodal block, the distal cells are similar to those in the proximal bundle branches.Branches from the anterior descending and posterior descending coronary arteries supply blood to the superior ventricular septum, making the conduction system at this site less susceptible to ischemic injury, unless ischemic Spread.
1.5. Branches of the bundle of His
The bundle of His is a structure that connects to the distal portion of the atrioventricular nodal block that passes through the central fibrillar body and continues through the annulus fibers, where it is termed the unbranched portion as it penetrates the membranous septum. The connective tissue of the central fiber body and the membranous septum enclose the penetrating part of the atrioventricular bundle, which can introduce extensions into the central fiber body. The proximal cells of the infiltrates are heterogeneous and resemble those of the atrioventricular nodal block, the distal cells are similar to those in the proximal bundle branches.Branches from the anterior descending and posterior descending coronary arteries supply blood to the superior ventricular septum, making the conduction system at this site less susceptible to ischemic injury, unless ischemic Spread.
1.6. Endless Purkinjes
The terminal Purkinje fibers connect with the terminal ends of the bundle branches to form an interwoven network on the endocardial surface of both ventricles, which transmit cardiac impulses almost simultaneously to the entire right interior of the right ventricle. and left. Purkinje fibers tend to be less concentrated at the base of the ventricles and at the papillae. They penetrate only the inner 1/3 of the endocardium. Purkinje fibers are more resistant to ischemia than normal myocardial fibers.1.7. Distribution of atrioventricular node, bundle of His, and ventricular myocardium
The atrioventricular node and the bundle of His are surrounded by an abundant supply of cholinergic and adrenergic fibers with a higher density than that of the ventricular myocardium. The parasympathetic nerves to the atrioventricular nodal region enter the heart at the junction of the IVC and the inferior surface of the left atrium, abutting the coronary sinus opening.Autonomic nerve input to the heart exhibits a degree of "toward tilt", with the right sympathetic and vagus nerves affecting the sinoatrial node more than the AV node and the sympathetic nerves and The left vagus affects the AV node more than the sinoatrial node. The distribution of neural input to the sinoatrial and AV nodes is complicated by significant internal overlap.
Right atrial ganglion stimulation produces sinus tachycardia with little effect on atrioventricular nodal conduction, whereas left star ganglion stimulation typically produces a continuous and ectopic shift of the sinus pacemaker shortened AV nodal conduction time and refraction, but inconsistently with the SA node discharge rate. However, stimulation of the right cervical vagus nerve slows the discharge rate of the sinoatrial node, and stimulation of the left vagus nerve mainly prolongs AV nodal conduction time and refraction when present. face. Neither sympathetic nor vagal stimulation affects normal conduction in the His bundle.

Loạn nhịp tim ảnh hưởng đến sự dẫn truyền trong tim
2. Conditions and disorders affecting conduction in the heart
2.1. Arrhythmia affects conduction in the heart
The normal sinus rate of 60-100 beats/min at rest is affected by a number of factors, including autonomic nervous system input, medication, metabolic and electrolyte status, and medical condition. .The causes of sinus node and atrioventricular node dysfunction are as follows:
Increased automaticity: Fever, catecholamine release, stimulants, drugs, hyperthyroidism, idiopathic Decreased automatism: Increased sound Drug vasoconstriction, electrolyte abnormalities, obstructive sleep apnea syndrome (OSA), myocarditis, endocarditis, post-operative degenerative heart disease, fibrosis, regurgitation, rheumatic heart disease , neuromuscular disorders. Inherited forms of cardiac conduction disease are rare, but the discovery of disease-causing gene mutations has improved our understanding of the underlying processes that generate and propagate impulses.
2.2. Other disorders
Bundle branch block: A block in the Purkinje fibers on one side of your heart, causing an arrhythmia. Heart block: Impaired electrical signal between the atria and ventricles of the heart. Long QT syndrome (LQTS): Your ventricles contract and release too slowly, sometimes leading to fainting or sudden cardiac arrest. Premature ventricular contractions: The heart beats too early in the ventricles, causing the heart to beat rapidly. Sudden cardiac arrest: A serious malfunction in your heart's rhythm that causes your heart to stop beating, leading to death if not treated immediately.3. A few tips for a healthy conduction system
Many heart rhythm problems are the result of genetic factors. They may be related to the structure of your heart or other factors.But you can work to keep your heart's conduction system and your entire heart working properly by living a healthy lifestyle as follows:
Achieve and maintain a healthy BMI; Avoid secondhand smoke and quit smoking; Do not abuse drugs or prescription drugs; Limit alcohol intake or drink alcohol only in moderation; Eat a nutritious diet full of fruits, vegetables, and whole grains; Try to maintain at least 150 minutes of exercise per week; Manage stress with healthy coping techniques, such as talk therapy or meditation. In a nutshell, your heart is a pump that carries blood throughout your body. For each heartbeat, electrical signals travel through conduction pathways in the heart. It begins when your sinoatrial (SA) node produces an excitatory signal.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: my.clevelandclinic.org, emedicine.medscape.com