This is an automatically translated article.
Posted by Dr. Do Minh Hung - Head of General Surgery Department, Vinmec Central Park International General Hospital.Serious complications associated with laparoscopic cholecystectomy include biliary tract injury, biliary leakage, bleeding, and bowel injury due to patient choice, surgeon experience, and technical awkwardness. The primary type of heat-induced biliary tract injury may be unrecognizable intraoperatively and usually involves the common hepatic duct or the right hepatic duct.
According to a study that gathered data from 7 large studies with a total of 8856 cases of laparoscopic cholecystectomy, serious complications accounted for 2.6%. Bleeding complications accounted for 0.11-1.97%, abscess 0.14-0.3%, biliary leak 0.3-0.9%, biliary tract injury 0.26-0.6% and intestinal injury 0.14-0.35%. The rate of wound infection with laparoscopic surgery was lower than with open surgery, but there was no difference in the incidence of abdominal abscess.
1. Experience of the surgeon
The overall complication rate is related to the surgeon's experience. A report of 8,800 cases of laparoscopic cholecystectomy performed by 55 surgeons, estimated a 90% biliary tract injury rate in the first 30 cases per surgeon, with rates down from 1.7% in the first case down to 0.17% in the 50th case. In studies, the rate of biliary tract injury accounted for 0.4 - 0.6%, 4 times higher than open surgery.
Experienced surgeons have the lowest complication rates. Today, laparoscopic cholecystectomy is almost routine, many hospitals that are now, and will be using this technique will require a certification of practice from a qualified training center. In the United States, the American Society of Surgeons, the Society of Laparoscopic and Gastrointestinal Surgeons have established a tool for evaluation called "Fundamentals in Laparoscopic Surgery (FLS"). ) and is required in the American Board of Surgery's review of qualified individuals to practice surgery.
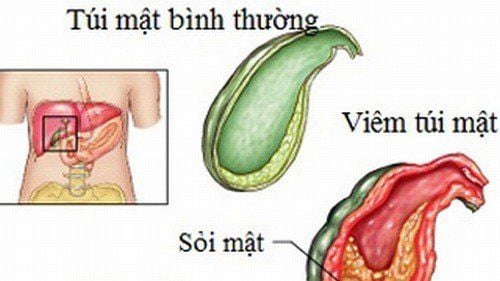
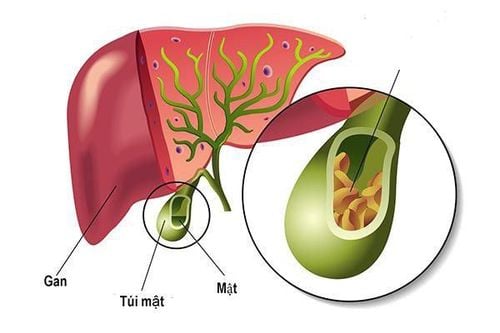
2. Inflammation of the gallbladder
Inflammation is also a determining factor in the risk of complications. Serious complications are often seen in patients with acute cholecystitis or chronic cholecystitis with sclerosing gallbladder wall or hilar adhesions. In cases like this, if the surgeon is not experienced enough and confident, the decision to switch to open surgery will be safer for the patient.
Trường hợp viêm túi mật cấp có thể ưu tiên lựa chọn phương pháp mổ mở an toàn hơn cho bệnh nhân
3. Injury to the biliary tract
Clinical manifestations of biliary tract injury vary widely, from asymptomatic biliary fistula that resolve spontaneously to complete obstruction of the extrahepatic biliary tract presenting acutely within a few days. Biliary obstruction in one lobe of the liver may not manifest for many years after laparoscopic cholecystectomy.
Biliary tract lesions can be detected at the time of surgery. If the surgeon has experience in biliary surgery, they will switch to open surgery to repair the lesion. In the absence of experience, they will invite a specialist in biliary surgery to manage the injury. A very small number of surgeons can repair these lesions with laparoscopic surgery.
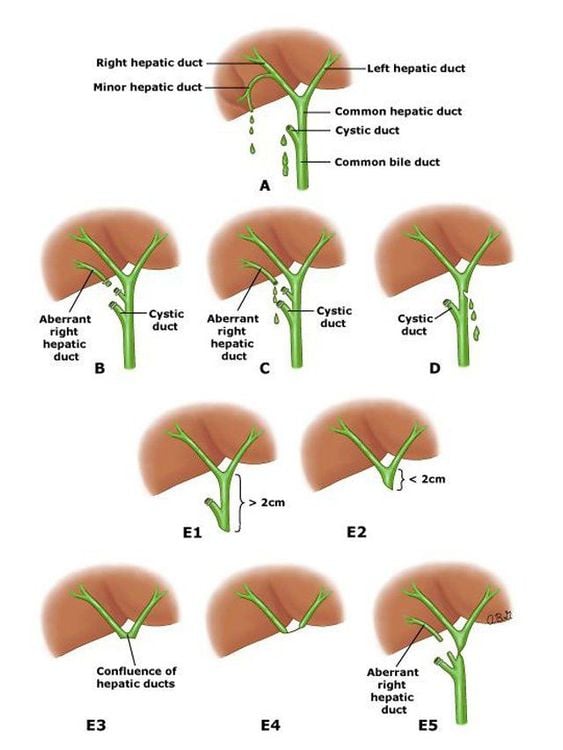
Hình ảnh đường mật bị tổn thương trong trường hợp khác nhau
4. Complications of bleeding
Complications of uncontrolled bleeding from laparoscopic cholecystectomy accounted for 0.1-1.9% and occurred in 3 prominent sites: liver, artery and trocar site.
Significant bleeding from the liver bed is quite common and is now considered to be due to the medial hepatic vein and its origin being too close to the gallbladder fossa, up to 10-15%. Bleeding usually occurs at the time of cholecystectomy from the gallbladder bed and if initial laparoscopic hemostasis is unsuccessful, conversion to open surgery should be performed for hemostasis.
Arterial control problems involving the cystic artery are immediately identifiable and controlled with clipping. The condition can also be acute hypotension immediately after surgery requiring resuscitation, blood transfusion and often re-operation. The culprit is usually a slipped artery clip.
The incision and the trocar site may bleed. Patients often have subacute manifestations in the first days after surgery. Some patients have delayed bleeding presenting with a hematoma seen on ultrasound as a heterogeneous hematoma. If the ultrasound is not detected, the diagnosis can be made by CT scan. If the patient is hemodynamically unstable, repeat laparoscopy for evaluation.
5. Intestinal damage
Is a complication caused by accident. If detected during surgery, this lesion can be treated immediately endoscopically if possible.
Patients may present with trocar site pain, abdominal distention, diarrhea, leukocytosis, and infectious cardiovascular collapse within 96 hours of surgery. If the patient has an infection or free air in the abdomen, immediate reoperation is required.
Phẫu thuật cắt túi mật nội soi có thể xuất hiện nhiều biến chứng