This is an automatically translated article.
The article was professionally consulted by Dr. Le Duc Hiep - Internal Medicine and Cardiovascular Interventionist - Cardiovascular Center - Vinmec Times City International HospitalAcute coronary disease, or the technical term is Acute Coronary Syndrome, is an acute medical condition, which is one of the most common clinical situations in practice. If not treated promptly, it can lead to life-threatening complications.
1. Complications of acute coronary disease
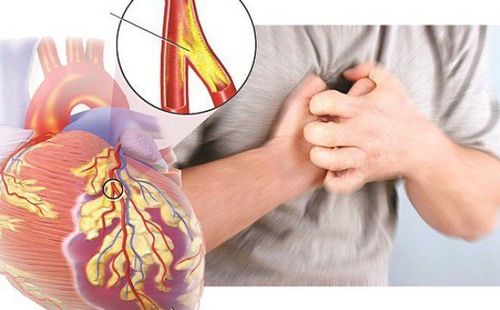
Acute coronary artery disease or myocardial infarction is the result of a blockage of the blood vessels supplying the heart (coronary system), often associated with atherosclerosis, causing myocardial necrosis - irreversible death.
As a result, heart function is severely affected and leads to dangerous acute coronary complications, even death. Basic acute coronary complications include:
Cardiac electrical function abnormalities such as arrhythmias or conduction disturbances; Abnormal mechanical function including: heart failure, heart rupture, acute valve regurgitation due to prolapse or rupture of the musculoskeletal ligament of the heart valve, apical aneurysm Formation of blood clots, blood clots in the chambers of the heart, especially in the case of heart failure. Severe heart disease or complications of apical ventricular aneurysm in myocardial infarction Secondary inflammatory reactions such as pericarditis, Dressler syndrome...
Of the complications of acute coronary artery disease mentioned above, the majority are cardiac electrical abnormalities, occurring in more than 90% of cases. These are complications of dangerous coronary artery disease, which can be life-threatening in the first 72 hours after the onset of infarction with manifestations: arrhythmias from a fast or fast enough rhythm, decreased cardiac output, hypotension blood pressure or bradyarrhythmias such as 2nd degree or higher atrioventricular block.
The most dangerous patient can enter a ventricular tachycardia (VT), ventricular fibrillation (VF) causing cardiac arrest. Cardiac arrhythmias may be caused by myocardial necrosis or by disturbances following myocardial infarction (including respiratory failure, electrolyte disturbances, etc.).
1.1. Sinus node failure This is an acute coronary complication that occurs when the coronary branch that supplies blood to the sinus node is blocked. Besides the signs of a heart attack, the patient's heart rate will slow below 60, maybe even less than 50 times / minute. In particular, complications of acute coronary artery disease in the form of sinus node failure are likely to occur in the background of patients with previous sinus node failure (common in the elderly).
Among the types of sinus node failure, the most common is simple sinus bradycardia. If the heart rate is still above 50 beats/min, there is no indication for treatment, besides this heart rate can reduce myocardial work and inadvertently reduce the degree of myocardial ischemia. More severe when there is a drop in blood pressure or heart rate less than 50 beats / min requires support with some drugs or a pacemaker.
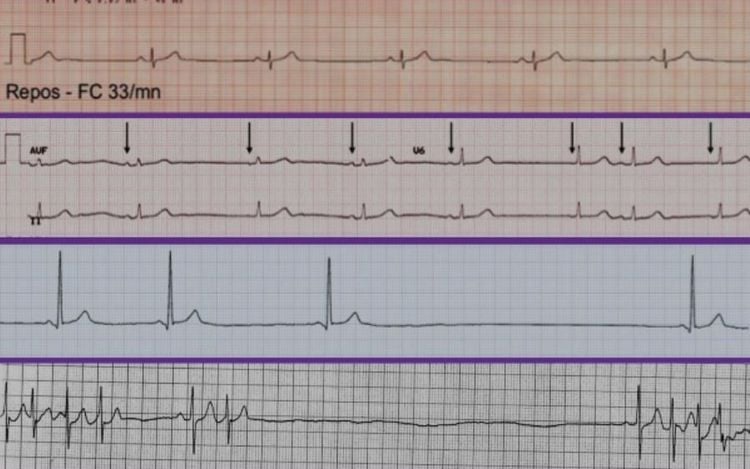
Hình ảnh suy nút xoang trên kết quả ECG
1.2. Atrial arrhythmias Atrial arrhythmias are an acute coronary complication that occurs in approximately 10% of patients after myocardial infarction. If left untreated, it can lead to left ventricular dysfunction or right atrial infarction.
Paroxysmal atrial tachycardia episodes are uncommon, more likely to occur in patients with a previous history of this condition; Atrial extrasystoles: Most are benign, but may also suggest concomitant heart failure if the number of extrasystoles is increased; Transient atrial fibrillation is a complication of acute coronary disease that occurs within the first 24 hours after infarction. Patients with factors such as age over 70 years, heart failure, large-scale myocardial infarction or atrial infarction, pericarditis, electrolyte disturbances... increase the risk of atrial fibrillation. Chronic or recurrent atrial fibrillation has a poor prognosis and increases the risk of thrombosis in the heart. 1.3. Atrioventricular conduction disturbances The most common acute coronary complication that causes conduction disturbances is atrioventricular block. Of these, first-degree atrioventricular block, or Mobitz I second-degree atrioventricular block, is quite common in anterior or posterior inferior wall infarction and rarely progresses to higher-grade block.
Mobitz II second-degree atrioventricular block and complete third-degree AV block are less common but more dangerous. Third degree atrioventricular block is related to the site of the infarct, occurring in about 5-10% of anterior infarction cases.
1.4. Ventricular arrhythmias Common ventricular arrhythmias, this may be a complication of hypoxemia, electrolyte disturbances or ischemic myocardium adjacent to the infarct with excessive sympathetic activity to compensate. . Common types of ventricular arrhythmias include:
Ventricular extrasystoles are very common after myocardial infarction and usually do not require treatment. Ventricular tachycardia of less than 30 seconds and even more prolonged but hemodynamically normal ventricular tachycardia does not require intervention for the first 24 to 48 hours. Varicose ventricular tachycardia, lasting more than 30 seconds, or any type of ventricular tachycardia with signs of hemodynamic instability, requires treatment with synchronized electroconvulsive shock. Ventricular fibrillation occurs in 5-12% of patients, occurring within the first 24 hours of myocardial ischemia. This is a complication of acute coronary disease with a poor prognosis, requiring immediate emergency treatment with asynchronous electric shock. 1.5. Heart failure When myocardial infarction is large or mechanical acute coronary complications occur, diastolic dysfunction will easily lead to heart failure. The severity of heart failure is closely related to the size of the infarct, the increase in left ventricular filling pressure, and the degree of decrease in cardiac output. Patients are often fatigued on exertion, dyspnea, auscultation with moist rales and auscultation. Signs of hypoxia are common symptoms of heart failure.
Suy tim là một trong những biến chứng của bệnh mạch vành gây ra
1.6. Cardiac rupture Complications of coronary artery disease cause rupture of the heart at sites such as the interventricular septum or free wall, the incidence is less than 1%. Especially, this is a very dangerous acute coronary complication, causing about 15% of patients to die at the hospital.
Rupture of the interventricular septum is about 8-10 times more common than rupture of the muscle column. Patients present with symptoms such as a loud T1 sound spreading from the apex along the left sternal border in the 3rd or 4th intercostal space, hypotension, or impaired left ventricular function. Complications of free wall rupture increase with age, and are more common in women. Characterized by sudden loss of arterial blood pressure while sinus rhythm is still present. Most are fatal, rarely prompt surgery.
1.7. Cardiogenic shock Hypotension or cardiogenic shock occurs when the left ventricle has decreased filling and inability to contract secondary to a large-scale myocardial infarction. Cardiogenic shock occurs when systolic blood pressure is below 90mmHg, tachycardia and signs of multi-organ failure such as decreased urine output, decreased consciousness, sweating, cold limbs...
About 5-10% of people The disease occurred with acute coronary complications in the form of cardiogenic shock.
1.8. Pericarditis Pericarditis is a complication of acute coronary that occurs in cases where the infarct has spread through the myocardium to the pericardium. Occurs in approximately one-third of patients with transmural myocardial infarction and decreases in frequency in patients treated with early reperfusion.
2. How to prevent complications of coronary heart disease
In order to reduce the complications of acute coronary disease, the first and most important thing is that the patient should be transferred to a medical facility with a full range of interventions or surgery to revascularize (thrombolysis). , coronary stenting or coronary artery bypass grafting) this is a key issue in treatment and improves the mortality prognosis for patients. Patients need to strictly follow the doctor's treatment instructions, take the right dose, and do not quit on their own. In particular, dual antiplatelet drugs are very important in the prevention of complications. In addition, the patient will be optimally controlled for risk factors such as: quitting smoking, controlling blood pressure, controlling blood sugar, blood lipids, ... besides changing the diet, changing the diet. lifestyle habits to contribute to reducing cardiovascular risks and beneficial to heart health.

Khám sức khỏe định kỳ giúp người bệnh phát hiện bệnh lý sớm bệnh lý tim mạch
3. When to see a doctor?
When the patient has symptoms such as severe chest pain or severe chest pain, shortness of breath, fatigue. In particular, the above symptoms occur in an acute, sudden way. Early examination and consultation with a cardiologist can help you get the earliest diagnosis and reduce complications for the patient.
For patients with high risk factors such as smoking, drinking a lot of alcohol, being overweight, having diabetes, having dyslipidemia, especially in middle age, they should be examined and screened. coronary artery disease whether the patient has or does not have chest pain symptoms.
For patients discharged from the hospital after coronary intervention, patients need to adhere to medication and follow-up appointments according to the doctor's appointment. In addition, patients need to be corrected for underlying conditions such as diabetes, dyslipidemia, etc. Therefore, in order to manage a patient well after myocardial infarction, it is necessary to have a combination of treatment. by many specialists and active cooperation from the patient and family. The monitoring, management and early recognition of coronary artery disease complications is essential work to protect the health of patients. Currently, at the Cardiovascular Center - Vinmec Times City International General Hospital is implementing programs to examine, screen, manage, monitor and early recognize complications of cardiovascular disease in general and coronary heart disease. level in particular. The whole procedure is performed by a team of leading specialists and is closely coordinated with many specialties: Cardiology, Imaging, Biochemistry, Immunology, Endocrinology, Department of Nutrition ... to bring efficiency as well as ensure long-term health for patients. After going through the treatment phase, the patient will also be monitored and re-examined to determine the treatment or detect more acute coronary complications?
If you have a need for medical examination and treatment, you can go directly to Vinmec Times City International General Hospital or register for an online examination.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.