This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
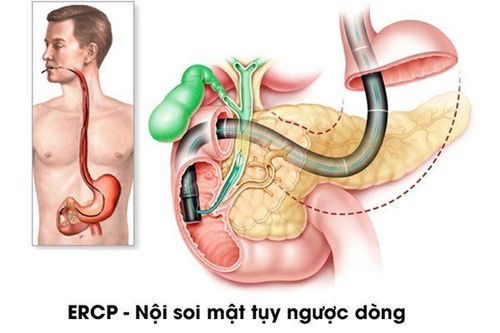
ERCP stands for "Endoscopic retrograd cholangio pancreatography", which means endoscopic retrograde cholangiopancreatography. ERCP is a procedure that can be used to diagnose and treat many different diseases such as gallstones, acute pancreatitis, and cholangitis.
1.Common applications of endoscopic retrograde cholangiopancreatography
Endoscopic decompression in acute pyelonephritis:
Emergency endoscopic biliary tract decompression can be indicated for patients in shock, coma due to biliary obstruction. Today, emergency endoscopic biliary drainage has reduced mortality in patients with pyelonephritis. Cholangitis is the most common disease caused by obstruction of the biliary tree. Usually secondary to gallstone disease and intermediate-stage infection. Due to the obstruction of the bile duct, the pressure is increased in the hepatobiliary branch, increasing the pressure inside the bile duct, leading to the reflux of bacteria into the hepatic duct, vein and allowing bacteria to enter the system. infectious circulatory system and its various manifestations.
Most investigations agree that, if a facility has the facilities and expertise in endoscopy, when a patient presents with acute cholangitis, the condition is more likely to lead to surgery. or radiographic intervention. Ideally, the patient should be medically stable and as stable as possible prior to endoscopic treatment with endotracheal anaesthesia. Although it is sometimes difficult to move patients and treatment equipment because this particular device is a bit cumbersome, endoscopy can be successfully performed in the operating room, which is equipped with an X-ray machine and has fluorescent screen. The success of endoscopy is due to a close working relationship with anesthesiologists who are available during endoscopy, a type of high-risk technique.
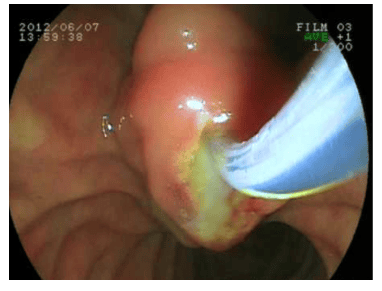
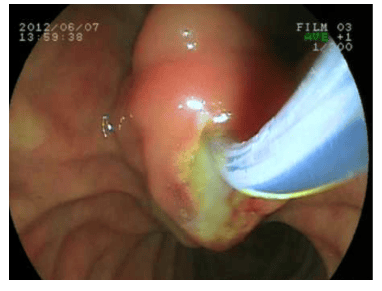
Paroxysmal cholangitis: Paroxysmal cholangitis (septic shock of the biliary tract) is a life-threatening disease that can be successfully treated with retrograde endoscopic techniques. All endoscopists are encouraged to hone their skills accurately to perform sphincterotomy quickly and efficiently despite the presence of infection and shock.
The risks of surgery should be carefully explained to the patient and family. From the experience of endoscopists, it is possible to save lives and reduce risks with physician support in primary care of biliary tract infections. Endoscopic treatment of acute gallstone pancreatitis: Previously, when talking about the causes of acute pancreatitis (acute pancreatitis), the causes that were not found were classified as innocuous. Today this concept has changed, the most common cause of acute pancreatitis is gallstones, followed by alcohol, and other less common causes such as metabolic, trauma, congenital malformations or parasites. parasites into the pancreas. The most commonly accepted etiology of acute pancreatitis is the “obstructive” theory. Pancreatic duct and bile duct are connected by a short passage before emptying into the duodenum, once there is a small gallstone running across and stuck in this joint, it will stop pancreatic juice and cause bile reflux. into the pancreas. It is due to this destructive effect of pancreatic enzymes that will cause acute pancreatitis.
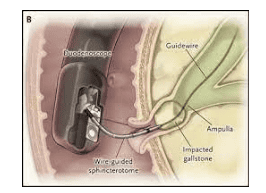
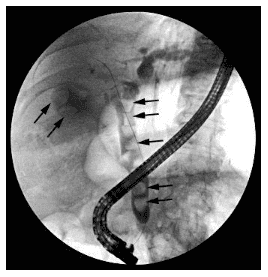
If the stone is passed, pancreatitis will go away and the chance of finding a stone stuck in the ampulla of Vater depends on the timing of the study. A series of surgeries revealed the presence of an entrapped stone even at the time of emergency surgery, just as a stone can be found with early endoscopy. The chance of finding a stuck stone gradually decreases after 72 hours, probably because the sphincter opens to allow the stone to escape into the duodenum. Another theory also proves that due to the reflux of duodenal juice into the pancreas at the moment when the large papilla (Papa Vater) opens to allow the stone to fall into the duodenum. Endoscopic retrograde cholangiopancreatography has been applied in the treatment of pancreatitis, especially in acute gallstone pancreatitis, it shows the biliary-pancreatic tract, detects gallstones, and removes the sphincter to remove OMC or trapped stones. in the ampulla of the liver and pancreas (the ampulla of Vater) is very effective and the disease recovers quickly. Also, parasites such as roundworm, a rare disease in Western countries that cause acute pancreatitis, can be obtained endoscopically without surgery. However, it is very important to note that endoscopic retrograde cholangiopancreatitis can cause acute pancreatitis by inserting a deep catheter or injecting too much contrast into the pancreas to make a diagnosis, especially in cases where the drug penetrates to the end. Islets or contrast material accumulates in pancreatic cysts. Due to excessive burning during sphincterotomy or the sphincterotomy knife entering the pancreatic duct without being checked by the endoscopist prior to resection, it may cause edema of the pancreatic opening and subsequently acute pancreatitis.
Intra-pancreatic cholangiopancreatosis: In the treatment of biliary-pancreatic diseases, the most common foreign bodies are primary bile duct stones, pancreatic duct stones, but another pathology is very specific in the heat area. That zone is roundworm on the bile duct, pancreatic duct, but through the world literature, data on endoscopic ascariasis is only found in a few reports. Mallet Guy and Maillet in 1945 reported to the French medical community about complications caused by roundworms. Gasparini et al. was the first Italian author to describe the symptoms of bile duct worms on radiographs in 1954. Fruchaud in 1957 reported a number of clinical reports of worms about this dangerous complication. According to Olivier, until 1960 a total of 40 medical records of biliary tract parasites were reported in the world literature, in which roundworms were the most common cause.
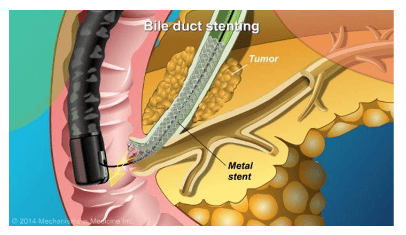
Endoscopic biliary decompression: The technique of catheterization of the biliary tract or pancreatic duct was first described in 1979. Since then, catheterization has been an accepted and applied method for the treatment of obstructive jaundice. due to malignancy, postoperative bile ducts, biliary stricture, pain in chronic pancreatitis, drainage of pancreatic pseudocyst. It is most commonly used for pancreatic cancer patients because only 10% are operable and the 5-year survival rate is less than 1%.
Perform diagnostic endoscopy and determine the extent of biliary obstruction, which can be ordered without sphincterotomy or minimal sphincterotomy can be performed in cases of large-sized catheters. The success rate of barrel placement ranges from 60-90% depending on the author as well as on the degree of narrowing. The degree of success was often higher in the group with strangulation of the middle third of the common bile duct as well as with low bile duct obstruction due to pancreatic head cancer. The failure was due to the tumor compressing much, deforming the duodenum, deviating the duodenal papilla, unable to insert the guide wire into the biliary tree to place the tube. Similarly, endoscopic nasogastric drainage is also widely used. In emergency situations, serious illness because of being infected with biliary tract, if surgery is not beneficial for the patient, endoscopic sphincterotomy and stone removal must be carried out for a long time, so endoscopic drainage of the nasogastric tube is recommended. A technique that is both gentle and effective, in some situations it may be possible to insert a biliary catheter as an alternative to a nasogastric tube.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.