This is an automatically translated article.
Article written by Orthopedic Doctor - Department of General Surgery - Vinmec Central Park International General Hospital
Cervical spondylosis can cause dangerous complications if not diagnosed, definitive treatment of the disease can seriously affect health and even affect the patient's life. Early identification of the cause of cervical nerve compression increases the likelihood of treatment by up to 80%.
1. What is cervical spondylosis?
Cervical spondylosis is a common disease, they cause a lot of pain and discomfort, reducing the patient's mobility.
This is a pathological condition related to the degeneration of the cervical vertebrae due to many causes. The disease is most common in the elderly due to the aging of the bones and cartilage in the cervical vertebrae. However, the disease can also occur at other ages if a cause is present. Currently, cervical spondylosis is tending to be rejuvenated due to many habits of young people.
Thoát vị đĩa đệm đốt sống cổ
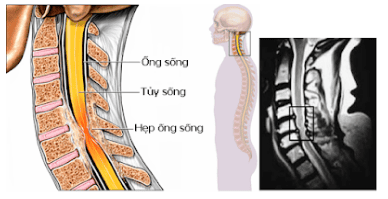
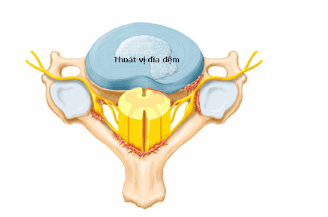
Normally, as we age, the spinal discs also gradually lose water, decrease in height, protrude and become stiffer. At that time, the adjacent vertebrae bodies press together, creating bone spurs around the disc to increase its stability. But these degenerative bone spurs also limit movement of the cervical spine, narrow the foramen junction and compress the nerve roots, causing neck - shoulder pain down the arm - hand.
2.Symptoms of cervical spondylosis
When the nerve root is compressed in the neck, it will cause the patient pain from the neck to the shoulder, arm according to the distribution of the damaged nerve root (diagram above). Accompanied by sensory disturbances such as stinging, numbness.
Patient may have weakness, paralysis of the arm. These symptoms may be aggravated when the patient performs movements such as stretching the arms, stretching the neck muscles, turning the head. Often the patient is more comfortable with the arm above the head and shoulder stretch.

Dấu hiệu thoái hóa đột sống cổ
3. Cervical spondylosis compresses which nerve?
Normally, the degenerative condition of the cervical spine compresses the nerve, which will directly affect parts such as:
Cervical nerve: In the neck, there are many blood vessels that are connected to each other; causing pain and numbness in the shoulder and neck area. Even when not moving, the pain is still painful, making the patient weak and tired. Cervical and Brachial Nerves: The hand part includes the wrists, arms, fingers and biceps that are connected by a tight, complex nervous system. When the nerve in any part is damaged, there is also the risk of affecting the entire hand area. When suffering from this disease, most people will feel pain, itching, loss of sensation, difficulty in grip and even muscle atrophy if not completely cured.
4.Diagnosis of cervical spondylosis
After the patient is asked carefully about symptoms, disease progression, the patient is checked by the doctor for movement, sensation, reflexes and cervical spine tension tests. Find movements and positions that cause pain according to nerve root distribution as well as positions that help the patient relieve pain. From there, it helps to make an initial assessment of the location and extent of the lesion, towards the implementation of a number of subclinical indications to help accurately diagnose the disease and choose a treatment method.
Tests to support the diagnosis of cervical spondylosis include:
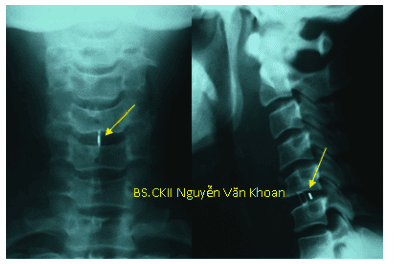
4.1 X-ray. Helps to evaluate the physiological curve of the spine, can see degenerative bone spurs, disc stenosis, and foraminal stenosis.
4.2 Computed tomography (CT Scanner) For more detailed images, bone spurs can be seen, especially at the foramen fusion.
4.3 Magnetic Resonance Imaging (MRI) Clearly shows the structure of nerve roots, spinal cord, discs. Shows which nerve roots are compressed, the degree of compression. Help the doctor locate the lesion for precise surgery.
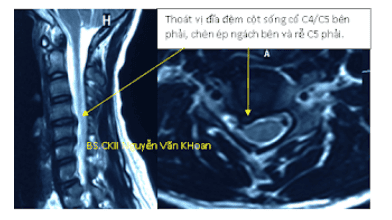
Chụp cộng hưởng từ thoát vị đĩa đệm cột sống cổ C4/C5 bên phải
4.4 Electromyography and nerve conduction Helps to distinguish symptoms of nerve compression from nerve damage caused by other medical conditions such as diabetes.
5.Treatment of cervical spondylosis
Many cases of patients with mild cervical radiculopathy tend to subside over time, without surgery, even without any treatment.
Some patients have pain that disappears on its own after a few days or weeks, others have persistent pain. Many cases of the disease recur after a period of time and can also go away on its own without treatment. In some patients, pain in the neck, spreading to the shoulder and arm, gradually worsens and may be accompanied by limb weakness that requires examination and treatment.
5.1 Conservative treatment When the patient has no severe pain and no complications of paralysis, apply:
Soft neck brace: Helps the neck muscles to rest and limit movement. This reduces nerve compression in the neck during movement. Only wear it for a short time when it hurts, because wearing it for a long time will weaken the neck muscles.
Physiotherapy: Helps patients relieve neck muscle tension, relieve pain, and strengthen muscle mass. It is possible to apply measures such as pulling the cervical spine, illuminating the lamp, exercising therapy ...

Điều trị thoái hoá đốt sống cổ theo phương pháp vật lý trị liệu
Medicines:
Non-corticoid anti-inflammatory drugs: Help relieve pain, reduce inflammation and reduce swelling of damaged nerves. Oral corticosteroids: Short-term use also reduces edema and pain. Sedatives: Only used for a short time for severe pain, unresponsive to other drugs. Intra-spinal injection: Corticosteroids are injected around the damaged nerve roots (e.g. epidural, into the foramen synovial or lateral joint) to increase the effectiveness of anti-inflammatory drugs. 5.2 Surgical treatment Indications for surgery when the patient's pain persists, worsens, and does not respond to conservative treatment. The goal of surgery is to decompress the nerve roots, stabilize the spine, and correct spinal alignment.
Surgical methods for cervical radiculopathy include:
5.2.1 Discectomy to decompress nerve roots and anterior intervertebral fusion This surgery is the most commonly used, to help decompress nerve roots. , create spinal alignment, intervertebral fusion (using PEEK wedge with or without bone graft, or using autologous bone graft taken from the patient's own iliac crest).
If only herniated disc in the cervical spine is 1 or maximum 2 floors, there are no other accompanying injuries such as degenerative spines compressing nerves, ossification of the posterior longitudinal ligament, spinal stenosis, spinal cord compression due to hypertrophy. large yellow ligament, congenital cervical stenosis ... then this surgery has a high success rate, few complications - complications.
Phẫu thuật cắt đĩa C5/C6 giải ép, đặc nêm PEEK lối trước. Sau mổ bệnh nhân hết đau, trở lại sinh hoạt bình thường sau 2 tháng.
5.2.2 Surgery to remove the nucleus pulposus, decompress the posterior nerve via endoscopic This is a difficult surgery, requiring a skilled, experienced and highly trained surgeon to perform. High risk of accidents if inexperienced, not skillful.
5.2.3 Enlargement of the vertebral plate and posterior fusion foramen Through the posterior midline longitudinal incision, part of the vertebral plate is resected and the foramen enlarged, the nerve root is decompressed without fusion. Through this incision, the nucleus of the hernia can be removed. Often used for cases of cervical spondylosis narrowing the foramen. However, it is also difficult to perform and is only applied narrowly to a few cases where the hernia is easy to retrieve.
5.2.4 Artificial disc replacement Remove the herniated degenerative disc tissue and replace it with an artificial, movable disc. This helps to keep the 2 vertebrae from becoming rigid and keeps the patient moving, while also preserving the natural curvature of the cervical spine. Performed through anterior incision. However, it is rarely used today due to many complications after a period of follow-up.
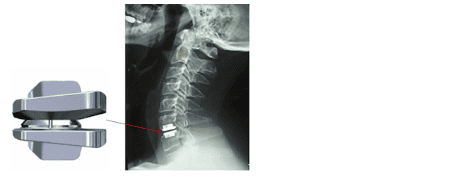
Thay đĩa đệm nhân tạo
5.2.5 Posterior vertebral plasty Apply in case of multi-stage disc herniation, with other associated injuries such as posterior longitudinal ligament ossification, spinal cord injury due to ligament hypertrophy yellow, congenital cervical stenosis.
Most cases of severe cervical radiculopathy can be resolved with surgery. However, the surgeon must be very careful and experienced, to avoid the risks of complications such as infection, bleeding, nerve damage, spinal cord injury, anesthetic reaction, epidural tearing, cerebrospinal fluid leak, oropharyngeal damage causing voice changes, difficulty swallowing after surgery... In some cases, patients did not improve their symptoms after surgery and sometimes had to undergo another surgery.
Rehabilitation after surgery: After surgery, patients are often advised to practice sitting and walking as soon as possible (in the first day), wear a soft or stiff neck brace for 4-6 weeks. Then have the patient practice neck movements. Patients can return to normal work after 3-4 months; Weld bone hardens usually after 6-12 months.
Vinmec Central Park International General Hospital is a prestigious address for examination and treatment of cervical herniated discs, highly appreciated by experts and trusted by many patients today.
The hospital focuses on investing in imaging equipment to support the most advanced diagnosis and treatment, giving clear images such as: G.E 3.0 CT scanner, CT SCAN Toshiba 640 slices, MRA and CTA... In particular, the team of musculoskeletal specialists at Vinmec Central Park are all well-trained in the country and many centers have the world's leading medical background, outstanding with translation services. comprehensive and professional medical examination, consultation and treatment services; a civilized, polite, safe and sterile medical examination and treatment space to help ensure the best quality of medical examination and treatment for patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.