This is an automatically translated article.
Care and treatment for amputation patients in the early stages is very important, starting from the first day after surgery until they are fully able to move in bed and move. safety around the patient room, at home and in surroundings. Let's learn more about amputee care after amputation in the article below.
Regardless of the reason, the loss of a limb is never easy. Both mentally and physically, amputation can negatively affect a person and is sure to change their life as well as the lives of their loved ones. Life after amputation is simply about finding a new habit - a new normal.
1. The amputated part of the leg and arm
1.1 Legs
Feet : Transverse amputation of the foot or ankle bone, ankle joint dissection. Leg : The stump is located between the upper 1/3 and the middle 1/3. The length is about 15 cm from the knee joint to the knee joint : Because the stump is too long, it will be indicated to remove the knee joint. Thigh : The stump is 25-30cm long. Hip : Indication to remove hip joint.
1.2 Hands
Hand : Disassembly of fingers and wrists Forearm amputation : The amputee is located at the middle and lower 1/3 position. Elbow : Dismantling the elbow Arm : The stump is in the middle 1/3 and upper 1/3 position. Shoulder : Remove shoulder joint
2. First time after amputation surgery
The first day after surgery is often the hardest as you process what was once a theory is now a reality. The wound will be bandaged and put on compression stockings, and may also be elevated or bandaged to help reduce swelling. Ensuring swelling and pain relief for the remaining limb is a top priority during this time. Proper treatment will make it easier to fit a prosthetic in the future.
Recovery will begin within a few days, but will primarily be very simple and gentle stretching exercises to help you maintain range of motion in all your other limbs. The physiotherapist may also teach you some exercises to prevent blood clots from forming.
Phẫu thuật cắt chi phải được chăm sóc cẩn thận
As before surgery, it is still important that you communicate any discomfort or concerns to the doctors and nurses in charge of your care. This includes any pressure points in the bandage or any pain in the residual limb.
The wound itself will take four to eight weeks to fully heal, but you will likely only stay in the hospital for up to 14 days. An extended hospital stay is to allow doctors to monitor your healing and monitor any conditions that may be hindering proper healing, such as diabetes or arteriosclerosis. circuit. They will also prescribe pain relievers and other medications to prevent infection.
Complications after amputation surgery Pain at the stump site: Due to the surgical scar against the nerve or pain in the adjacent part of the amputated limb, also known as "ghost limb" pain
Bleeding: Due to trauma The pulsation causes bleeding of the bone head or incomplete hemostasis, slipping only the constricted part of the blood vessel. In these cases, it is possible to apply pressure to stop bleeding, apply cold or may need to have surgery again
Osteomyelitis: Conservative treatment or re-surgery
Muscle abscess: Draining pus drainage, combined antibiotic treatment spot and full body

Sau khi mổ cắt chi, mỏm chi có thể bị tổn thương nếu như không chăm sóc cẩn thận
Dermatitis of the head and around the stump: It can be caused by an allergy to topical medications, bandages, or heat that causes blistering of the skin, then ulcers, or it can be due to poor hygiene care.
Boils deep in the soft tissue: Use a hot bag to reduce the size of the infected area, then dredge it and use a combination of antibiotics.
Loss of sensation: It is a very important problem because the patient cannot feel the pressured prosthetic limb, crushing the organization. If the area of loss of sensation is extensive, it may be necessary to re-amplify the limb at a higher position. If the area of loss of sensation is narrow, care should be taken when making a prosthetic limb.
Difficulties after amputation surgery Limits on living: Depending on the amputation location, it will affect the daily life and movement of the patient and family to a greater or lesser extent. If the position is in the foot, the patient can walk normally and gradually get used to daily activities. If the stump is in the hand, it will affect holding, bathing, cleaning, changing clothes...
Joint deformity and muscle contracture : The stump if not given physical therapy and placed in a good position Right, there will be shrinkage and deformation even muscle atrophy.
Psychology: Especially for women and those who are the main laborers in the family, psychology will be deeply affected. Or with children when they have to go to school, they will receive jokes from friends that feel embarrassed.
Study and work : If the case of amputation in the right hand will make it difficult for children to write. For adults, work will be significantly affected.
3. Care after amputation surgery
3.1 Incision
At the stump, the doctor will use a stapler or suture to fix the scalp of the stump. The stapler or suture will stay in place for 4-6 weeks, depending on the healing state of the incision. Your incision may feel thickened and raised. This is normal and should subside over time (6-12 months). Keep your incision clean and dry. Do not apply any creams, lotions, powders, or ointments to your incision unless told to do so by your doctor. Do not scrape your leftover skin as this may cause irritation. Keep your incision out of sunlight for 6 months for optimal effect

Chăm sóc viết mổ thật cẩn thận
After the incision heals, you may be asked to gently massage to reduce shrinkage of the scar tissue. Wear your shrink socks as directed to help reduce swelling in the rest of your limbs. It also helps shape the limb to fit your prosthetic. You will be fitted for a shrink sock (compression stocking) while in the hospital or later in time. Usually, shrink stockings are applied on the 2nd day after surgery if the incision looks good. In the shower:
Wash your incision daily with soap and water and dry, beginning 72 hours after surgery. Use freshly laundered towels and towels each time you shower. You can shower if you have been cleaned with physical therapy and appropriate safety equipment in place. Do not soak in a bathtub or hot tub or swim in a pool or lake until the incision is completely dry or with your doctor's approval.
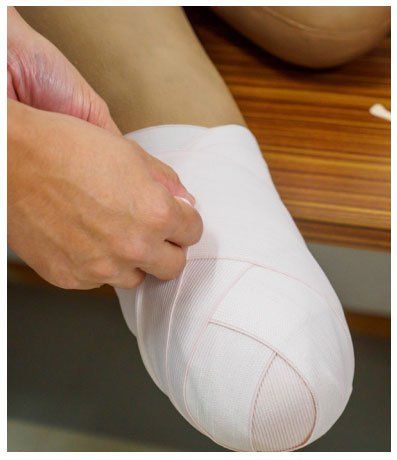
3.2 Amputation tape
Purpose:
Limit edema Firming soft tissue Enhance venous circulation Make the stump get used to regular coverage Soft tissue shaping Principle:
Do not use bandages that lose elasticity Restoration No horizontal bandage, but oblique or diagonal bandage The pressure of the bandage gradually decreases from the tip to the base of the limb The bandage should not restrict joint movement nor affect circulation, should not cause creases or folds on the skin Do not cause pain to the patient Do not let the bandage slip during the patient's movement Do:
Start when the stump is not stable, usually on the first day after surgery The stump must be cleaned. Clean before dressing Bandage should be sterile or cleaned and laundered daily. If edema is present, the stump circumference should be checked before and after dressing Bandage in the morning before the patient drops to bed. continue day and night without the prosthesis, even if there is no edema When the dressing should not leave wrinkles in the bandage Save Note:
The amputation of the upper limb is used with an elastic band of 8-10cm wide; The amputation of the lower limb is used with a 10cm wide elastic band; The amputation of the upper limb is used with a 15cm wide elastic band: Continuous elastic bandage, only no longer when the patient wears a prosthetic limb. Regularly If no prosthesis is worn, the stump needs to be bandaged, especially when the patient is often in a standing position with the lower extremity.
3.3 Correct posture
Placement of amputation on the knee Lie on your stomach immediately after surgery to avoid hip flexion deformation. Pillows should not be placed under the stump and sand bags should be placed along the outside of the stump to avoid deformation of the hip joint When lying on Bed: Turn at least every 2 hours from side to side. Keep the head of your bed at a 30-degree angle or lower to avoid putting too much pressure on your bones (hips when lying on your side, tailbone when lying on your back). Should lie flat on the bed, if the bed has a mattress, you should put an extra hard wood under the mattress because the soft mattress is easy to create folding deformation. It is not recommended to lie on the side, because in this position it is impossible to avoid the flexural deformation of the stump

Cần có tư thế đúng cho việc chăm sóc các viết mổ
Try to keep the thighs in a neutral position because in both the prone and supine positions, the patient tends to lie with the stump abducted and externally rotated. When sitting, change your position every 15 minutes by leaning forward or to the side so your lower body lifts off the chair. Stand up or perform “push-ups” using the arms to lift from the chair every hour Do not allow the patient to sit for a long time for the first 10 days after surgery with 90° hip flexion. Amputee position below the knee:
Place a pillow between your ankles and knees when lying on your side. Place a pillow under your shins to elevate your heels when lying on your back. The prone position reduces pressure on the coccyx, and due to the influence of gravity can further stretch the knee joint. The patient can be sat up early, but the coccyx must be kept in an extended position.
3.4. Positions to avoid for amputees above and below the knee:
Put a pillow under the hip or knee Letting the stump lie down on the side of the bed Sitting in a wheelchair with the stump flexed Lying on the back with the knee bent Lying with the knee bent Lie down with a pillow between the thighs Lie on the stump Stand up on crutches
3.5. Exercises to move the stump
Are exercises that serve many purposes, and are very simple. Applied in the stage before prosthetic part.
Effects brought from the exercises include:
The coccyx muscles are strengthened, especially the extensor, extensor and rotation muscles in the coccyx begin to get used to the pressure, ready for use Prosthetics Improve circulation Maintain flexibility in muscles and joints Increase muscle tone Get used to the muscle coordination needed by the stump to prepare for the use of prostheses Exercises:
Stand with parallel bars: Legs 20cm apart, alternately putting weight on both legs, both healthy and prosthetic. It is possible to change the exercise position to one foot in front and one foot in the back, constantly changing the weight on both legs. Practice walking in a bar parallel to the prosthesis: Walk slowly, slowly bringing the prosthesis forward. Practice standing and sitting with a high chair: Bend over with your weight forward and then stand up. Practice walking with parallel bars: Step your good foot to the side (right or left) and then follow the prosthetic leg. Fall practice: Put many thick pillows or wide cushions for the patient to exercise. So that when they fall, they will not have their whole body hit the ground. Practice falling forward, backward or sideways. Practice sitting down and standing up from the floor. Practice getting up from an assisted and unassisted kneeling position
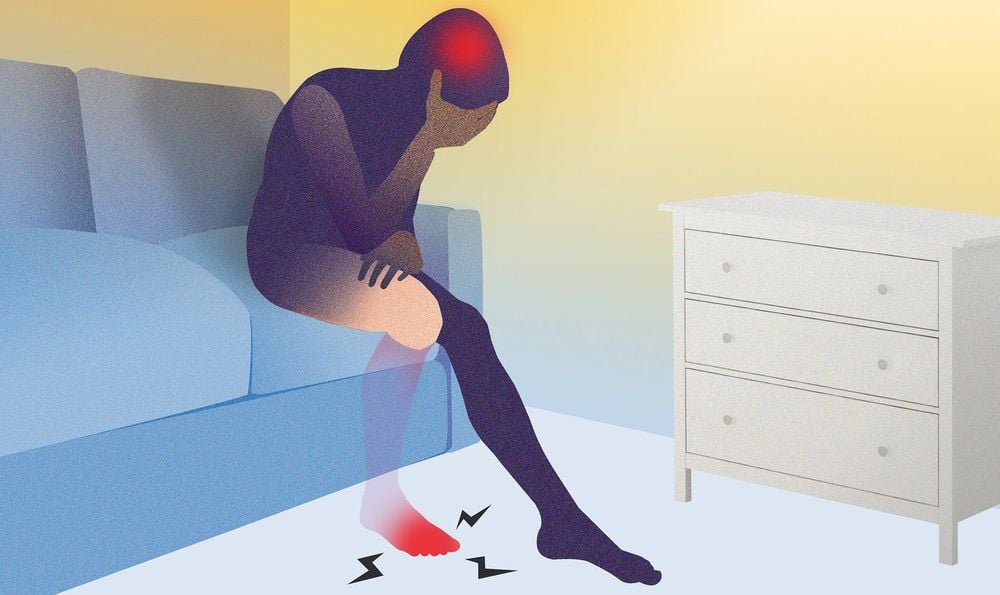
3.6. Get familiar with virtual limb syndrome
The most common psychological side effect of amputation is phantom limb syndrome, which is when you believe you can feel the amputated limb. Although most amputees feel like they can feel the amputated limb, not all of them feel pain there. The ghost sensation comes from the spinal cord and brain.
On the other hand, Phantom Pain remains a mystery. Theories about the cause of prosthetic limb pain suggest that it has something to do with brain reorganization after amputation. When a limb is amputated, communication between nerve cells in some nerves and the brain is disrupted. Eventually, those neurons are reactivated and begin to communicate with the brain again by responding to input from the nerves that are still present. Sometimes, putting pressure on the residual limb is what triggers this communication, causing the amputee to feel ghostly pain.
Both phantom pain and phantom sensation are common and tend to affect older amputees. It can develop soon after amputation or even weeks, months, or years later. Stress, anxiety, and fear are all potential triggers for phantom pain, and the pain itself can range from aching, cramping sensations to burning or shock.
Hội chứng chân tay giả thường sẽ diễn ra
Many people find that they no longer have prosthetic pain after wearing the prosthesis, but some home remedies can help alleviate the phantom pain, including:
Wrap the residual limb in a warm towel or heating pad. Apply ice cream or an ice pack to the residual limb. Massage the remaining limb and exercise the mind for the missing limb. Change positions by standing up or moving around. If you have a prosthetic, putting it on and going for a walk can sometimes help with lower body amputation. Tighten and slowly relax the muscles of the other limb.
4. Ways to deal with amputations
The mental impact of amputation can be very serious and there is no way to deal with your amputation. Grief, anger, depression are just some of the emotions you're likely to feel - and they're all valid and normal. What's important is how you deal with these feelings, whatever they are.
Here are some healthy ways to deal with amputation:
Accept and acknowledge your feelings: Whatever your feelings are, don't ignore them even negative emotions. Acknowledging good and bad feelings is the first step in dealing with them. Instead of forcing yourself to stay optimistic, allow yourself to be sad or angry if that's how you feel - and remind yourself that you're allowed to feel that way.
Focus on the journey : Rehabilitation after amputation has no timeline. It is different for everyone and can take years. Emotional recovery is often a lifelong task, so focusing on the end goal is rarely helpful. Instead, learn to appreciate your progress so far and try not to obsess over how far you have to go.
Find purpose: Whether it's spiritual, selfless or just fun, find something that excites you when you wake up in the morning. Some people enjoy volunteering with organizations that help amputees while others have a hobby to own. Whatever it is, just make sure it makes you happy to be alive and working on your recovery.
Learn to think about yourself in a new way : Instead of focusing on what you can't do anymore, try to focus on everything you can still do - and have learned how to do since the amputation foot. Reframing the way you see yourself can boost your mental health and confidence, and help normalize amputations for others.
Talk to other amputations : No matter how well-intentioned your loved ones and rehabilitation team are, they won't understand how you feel. People with similar backgrounds will be able to share more of their experiences, and they may also be able to provide relevant coping mechanisms that are not known to people without amputation.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.