This is an automatically translated article.
Posted by Doctor Pham Thi Hai Yen - Rehabilitation Department - Vinmec Times City International Hospital
Rehabilitation plays an important role for stroke patients, it should be done early in a rich movement and activity environment with the long-term goal of helping patients after a cerebrovascular accident perform the following tasks: perform daily activities as independently as possible, with basic skills such as eating, dressing, walking...
1. Common complications in stroke patients
There are many complications and sequelae that are common after stroke and improve over time depending on the extent of the disease, the course of treatment and rehabilitation.
Movement disorders: weakness, partial or hemiplegia, facial paralysis. Cognitive disturbances, reduced thinking, mild to severe memory loss, intellectual decline. Circular muscle disorders: urinary or bowel incontinence. Can cause bladder infection by inserting a urinary catheter. Language disorders: slurred speech, slurred speech, altered intonation, difficulty expressing thoughts in words, even failure to speak Visual disturbances.
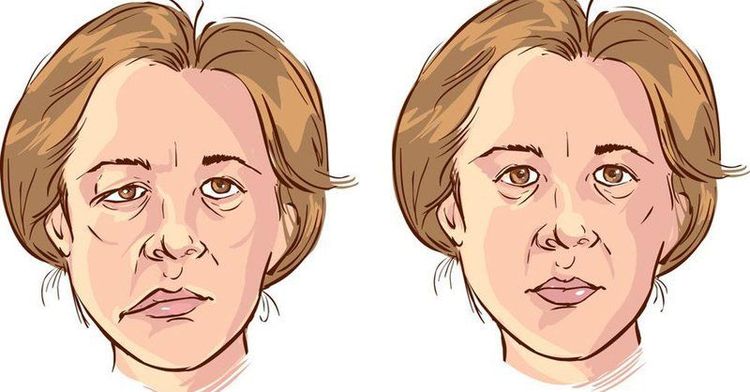
Liệt mặt do chứng đột quỵ gây ra
Sensory disturbances: pain, numbness, or burning and tingling sensations. I can't even feel a part of my body. Fatigue, balance disorder, insomnia or sleeping too much... Difficulty swallowing, difficulty swallowing combined with paralysis can lead to pneumonia due to food and drink entering the lungs. Ulcers in pressure areas due to long-term paralysis. Decreased social skills, daily personal activities. If the above disorders are not treated for a long time, resulting in the patient not being able to take care of themselves, having to depend on others, increasing the burden on relatives and family, the patient easily falls into a state of depression. depression .
2. Rehabilitation care measures to do
Rehabilitation is extremely important for stroke patients. It should be done early in a dynamic, activity-rich environment with the long-term goal of helping patients after a stroke to perform daily activities as independently as possible with basic skills. such as eating, dressing, walking...
Based on principles:
Prevention of respiratory complications. Encourage placement of therapeutic positions Early mobilization Maintain range of motion

Bệnh nhân tập phục hồi chức năng sau đột quỵ
Treats hemiplegia/hemiplegia Treats loss of sensation Facilitating upper limb function Strengthens muscle strength Improves gait, balance and mobility Encourages independence and daily activities Handles and Prevention of Common Complications of Stroke 2.1 Prevention of Respiratory Complications: Roll over often Therapy position (complete supine lying is not recommended as it may adversely affect air circulation and safe swallowing). Encourage regular deep breathing exercises. Encourage mobility (if medically stable). 2.2 Positioning therapy aims to facilitate optimal recovery after stroke through: Controlling muscle tone Increased spatial awareness Rolling over, changing position every 2 hours prevent pressure ulcers. 2.3 Promote mobilization early and as much as possible in patients with well-controlled medical conditions. In the acute phase after a stroke, people are at increased risk for complications from immobilization, such as muscle weakness, breathing problems (such as respiratory infections, pneumonia), pressure ulcers, and decreased blood pressure. joint range of motion, contractures, decreased general well-being (decreased cardiopulmonary endurance), thrombotic complications (eg, lower extremity deep vein thrombosis, pulmonary embolism) and osteoporosis.
The psychological effects of early mobilization may also help reduce depression and reduce the cost of care.
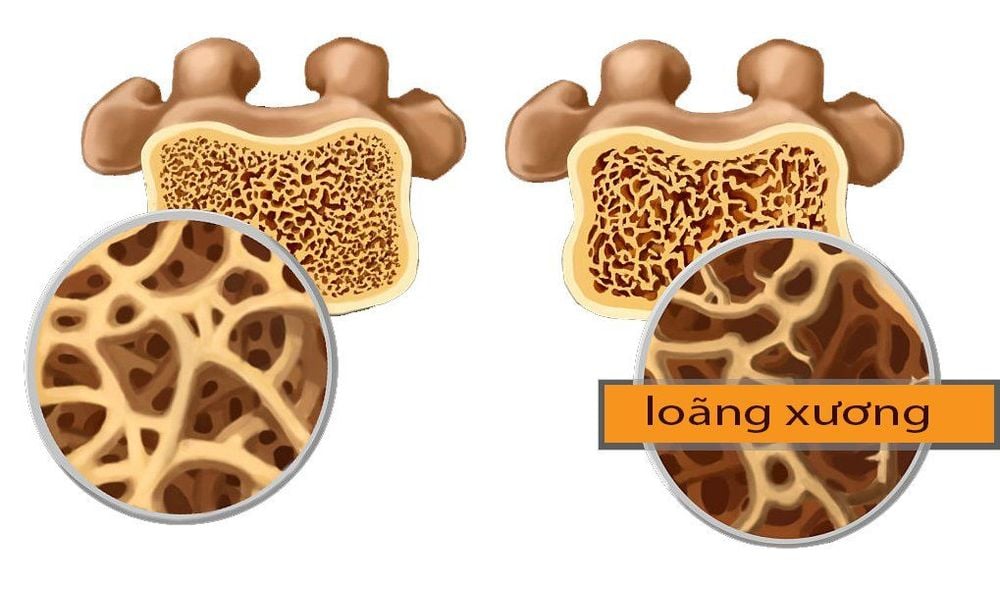
Người bệnh dễ có nguy cơ mắc bệnh loãng xương
Depending on the medical stability of the patient with a motor stroke, it can be:
Rolling over in bed Making a bridge Sitting up in bed Switching from lying down to sitting with legs dangling on the edge of the bed Sitting outside of bed Standing and walking 2.4 Maintaining range of motion of joints 2.5 Treatment of hemiplegia in the early stages often reduces muscle tone. Passive range of motion exercises and correct posture reduce complications of muscle weakness, contractures, and trauma to the paralytic side, and normalize tone and muscle strength in the paralytic side. Use your good hand to actively practice helping the paralyzed hand. Encourage active, functional exercises such as reaching for a cup, combing hair, etc.

Tập vận động liệt nửa người giai đoạn đầu trên bệnh nhân đột quỵ não
2.5 Handling of loss of sensation: the aim is to avoid injury to the patient, to assist in paying attention to the paralyzed side to restore sensation. Use massage/stroking techniques on the paralyzed side with different materials. Regular exposure to specific sensations can be practiced if the patient is tolerable, e.g. exposure to various materials, temperatures and pressures. 2.6 Facilitating upper extremity function to encourage independence and provide motivation to aid recovery Instruct the patient in exercises for the weak arm, using functional activities as much as possible is the practice of sitting or standing, e.g. bringing a cup to the mouth, moving objects from one place to another. ▪ Neuromuscular electrical stimulation: treatment by medical personnel. Virtual reality training of the paralyzed lateral arm and hand in stroke patients as an adjunct to routine exercise. Robotic-assisted exercise for paralyzed shoulder and elbow in stroke patients.

Kỹ thuật viên hướng dẫn người bệnh các bài tập với tay yếu liệt
2.7 Wrist and hand splints: prevention of neck - table - finger contracture in spastic paralysis cases. 2.8 Strengthens muscles to encourage independent recovery of motor function. Gradually increase muscle strength by increasing repetitions of weight-bearing activities (eg, repetitive sitting-to-standing transitions). Exercise with weights. Resistance exercise with machines such as stationary bikes. Strength training in the paralyzed leg or both legs in stroke patients has been shown to increase muscle strength and resistance during passive movement, and improve stride rate, symmetry, and step length. foot of gait.
2.9 Improve gait, balance and mobility to encourage independence, psychological support and motivation and endurance training. Practice balance. Guiding the correct gait. Use an assistive device such as a cane or AFO splint if appropriate. Practice walking and going up and down stairs, walking on different surfaces. Exercise with a weight-supported treadmill. Robotic-assisted gait training 2.10 Encourage independence and daily activities.
3. Rehabilitation of complications after stroke:
Shoulder sub-dislocation: to prevent shoulder sub-dislocation and pain due to decreased muscle tone and paralyzed shoulder muscles, stroke patients are placed in correct upper limb posture, using shoulder support devices such as shoulder belts , treatment of electrical stimulation of the deltoid muscle. Cardiopulmonary Endurance Loss: Cardiopulmonary endurance is significantly reduced due to immobility in the early stages of a stroke. Exercise, cycling, walking ... are rehabilitation methods to increase cardiopulmonary endurance, encourage patients to participate in regular and continuous exercise. cardiopulmonary endurance exercise program.
Fatigue after a stroke is unrelated to previous levels of exertion and usually does not improve with rest. These patients must be screened for depression, have reasonable exercise and rest time, create good sleep...

Người bệnh mệt mỏi sau đột quỵ cần được nghỉ ngơi hợp lý
Perceptual problems include amnesia on the paralyzed side and loss of awareness of objects with the senses and loss of awareness of objects when touched, rehabilitation methods:
Simple hints and reminders to draw attention to the paralyzed side. Paralyzed side movement. Practice eye scanning, eyeball movement combined with sensory stimulation of the paralyzed side through activity. Perform activities symmetrically on both sides of the body. Visualize images to enhance attention and use the forgotten side. Touching objects with different shapes, sizes, roughness... to stimulate sensations. Language and communication problems:
Teach the patient the words, phrases and gestures necessary to be able to integrate into community life. Use assistive devices such as hearing aids, communication boards, assistive chairs, etc. Encourage the patient, family/carers and community members to use other communication methods. such as gestures, facial expressions, speaking, reading, writing, drawing, using communication aids.

Người bệnh có thể được chỉ định dùng máy trợ thính hỗ trợ trong giao tiếp
Stroke is not only an acute condition but also causes long-term disability and sequelae. Therefore, stroke patients need appropriate and ongoing rehabilitation care, starting in a hospital setting during the acute phase, and proactively monitoring and supporting patients as they move through the subacute stages. and chronic when discharged home.
Currently, Magnetic Resonance Imaging - MRI/MRA is considered a "golden" tool for brain stroke screening. MRI is used to check the condition of most organs in the body, especially valuable in detailed imaging of the brain or spinal nerves. Due to the good contrast and resolution, MRI images allow to detect abnormalities hidden behind bone layers that are difficult to recognize with other imaging methods. MRI can give more accurate results than X-ray techniques (except for DSA angiography) in diagnosing brain diseases, cardiovascular diseases, strokes,... Moreover, the process MRI scans do not cause side effects like X-rays or computed tomography (CT) scans.\
Vinmec International General Hospital currently owns a 3.0 Tesla MRI system equipped with state-of-the-art equipment by GE. Healthcare (USA) with high image quality, allows comprehensive assessment, does not miss the injury but reduces the time taken to take pictures. Silent technology helps to reduce noise, create comfort and reduce stress for the client during the shooting process, resulting in better image quality and shorter imaging time. With the state-of-the-art MRI system With the application of modern methods of cerebral vascular intervention, a team of experienced and well-trained neurologists and radiologists, Vinmec is a prestigious address for stroke risk screening and screening. reliable goods.
In the past time; Vinmec has successfully treated many cases of stroke in a timely manner, leaving no sequelae: saving the life of a patient suffering from 2 consecutive strokes; Responding to foreign female tourists to escape the "death door" of a stroke;...