This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Tran Quoc Vinh - Emergency Doctor - Department of Resuscitation - Emergency - Vinmec Nha Trang International General Hospital.1. Hyperglycemia after surgery
Postoperative hyperglycemia occurs in approximately 50% of patients with or without pre-existing diabetes. Blood sugar regulation includes the impact of 3 factors that are:The balance of insulin and a group of antagonist hormones: Glucagon, cortisol, epinephrine. Neural factor control: glucose-sensing receptors in cells Liver regulation via autologous mechanism. Hyperglycemia after surgery is caused by many factors such as insulin resistance in the cells, insufficient insulin production or the body's response to stress, leading to insulin antagonist hormones such as cortisol, and catecholamines increased after surgery. Increased cortisol and catecholamines decrease insulin sensitivity, while elevated sympathetic activity reduces insulin secretion while increasing growth hormone and glucagon secretion. Severe or mild hyperglycemia depends on the duration, underlying medical conditions, inflammation and type of surgery,...
Surgery can lead to a number of metabolic disorders that can make blood sugar worse. Changes in the normal homeostasis of glucose lead to hyperglycemia. Hyperglycemia is a risk factor for postoperative infection, endothelial dysfunction, cerebral ischemia, and impaired wound healing. In addition, it causes other serious events in patients with underlying diabetes such as ketoacidosis (DKA), increased osmotic pressure (HHS) during and after surgery.
Many studies have shown a relationship between post-operative hyperglycemia with the rate of complications and mortality of patients. Controlling hyperglycemia is the primary goal of reducing the patient's ability to recover from surgery.

2. Control blood sugar after surgery
2.1 Goals of glycemic control after surgery Previously, hyperglycemia during surgery was considered a natural response of the body, patients need more energy to overcome the stress of surgery or disease disability. However, in a 2001 Leuven (Belgium) randomized controlled clinical trial that was performed in 1548 patients, between patients with tight glycemic control with a goal of 4.4 - 6 ,1 mmol/L and 10-11.1 mmol.L in the control group, showed marked improvement in mortality and complications in the group of patients with tight glycemic control.However, in a 2006 Leuven study and 2009 NICE-SUGAR study, tight control of blood glucose (4.4-6.1 mmol/L) did not change the incidence of complications such as: Infection, kidney failure,... even increased the rate of hypoglycemia and the risk of death higher than the control group (10-11.1 mmol/L)
With different study results, Currently, glycemic control in the range of 4.4-6.1 mmol/L during surgery as well as in resuscitation is no longer recommended. And associations and organizations such as the American Society of Clinical Endocrinologists, the American Diabetes Association, and the American Society of Outpatient Anesthesia agree to prescribe intravenous insulin therapy for critically ill patients if their blood sugar levels are high. blood >10 mmol/L (180 mg/dL). The goal of treatment is to maintain blood glucose between 7.8 and 10 mmol/L (140 to 180 mg/dL) and blood glucose levels should not fall below this threshold, especially <6.1 mmol/L (110 mg/dL). /dL).
In addition to hyperglycemia, control to avoid hypoglycemia is also an important goal, especially in patients who are being controlled with insulin. Because during surgery, patients can use anesthesia, sedation, muscle relaxants.., so the symptoms of hypoglycemia are often difficult to recognize. Periodic monitoring every hour by laboratory tests is recommended. Post-surgery patients still have side effects of anesthesia, sedation or need to use sedation as in the case of ventilator support, blood sugar monitoring should be checked periodically. set.
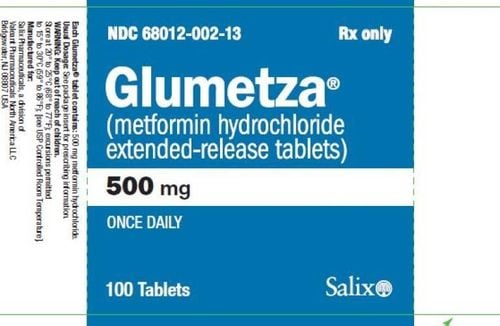
2.2 Methods of blood sugar control Most oral antidiabetic drugs have the risk of hypoglycaemia and are difficult to control. Intravenous or subcutaneous insulin therapy is the most ideal method to effectively regulate blood glucose including:
For non-insulin-treated patients: if capillary glucose is 4-12 mmol/L, no intervention is necessary. card. If glucose > 12mmol/L, intravenous maintenance insulin therapy can be given, then capillary checks are made regularly until stable. Discontinue IV insulin when the patient resumes eating and consider switching to subcutaneous insulin every 12-24 hours, then possibly switching to maintenance with oral hypoglycemic agents.

3. Caring for patients with hyperglycemia after surgery
Proper nutrition is extremely important for patients with hyperglycemia. Some of the nutritional guidelines include:3.1 Fasting phase During the postoperative fasting phase, patients with hyperglycemia will be controlled with subcutaneous insulin and monitored every 2 hours. try times. For patients with impaired consciousness or in need of intensive care, insulin should be administered intravenously.
Insulin regimen should include: slow basal insulin and rapid insulin to correct capillary blood sugar when the concentration is greater than 10 mmol/l. The insulin dose should be calculated on the basis of the presence or absence of pre-diabetes, the presence or absence of antidiabetic agents, frequency, dose, and route of administration. In patients who are not receiving parenteral nutrition or have very little intake, a slow insulin dose should be started at about 0.2-0.25 units/kg/day. In elderly and frail patients or with kidney disease, the dose should be reduced by half to limit the risk of hypoglycemia.
3.2 The phase of parenteral nutrition is too late The diet of patients with hyperglycemia after surgery should be divided into 3 main meals to reduce the amount of insulin secreted to serve the digestive process.
Starch: The complex starch group helps the body synthesize glucose slowly and steadily without causing a sudden increase in blood sugar after eating such as green vegetables, whole grains. . Animal proteins in red or white meat such as milk,... Fat: Fat group contains a lot of plant group such as unsaturated fat, helps to reduce serum cholesterol concentration such as avocado, nuts, soybean oil, olive oil,... Some foods should be avoided:
Starch: Simple sugar group found in foods with high content of natural sugar or artificial sugar, they suddenly increase sugar capillary blood. Foods containing a lot of simple sugars should be avoided such as: candy, soft drinks, sweet fruits, white bread, carbonated water,... Trans fats: Baked goods, margarine,... Cholesterol: Cholesterol is found in foods such as high-fat milk, liver, organs, high-fat animal protein, egg yolks, etc. Do not consume more than 200mg of cholesterol/day. In summary, care and blood sugar control of patients after surgery is essential to minimize complications, and improve surgical outcomes. In addition to the use of therapeutic drugs, patients need to pay attention to a reasonable diet to help control blood sugar easier.
Special note, it is necessary to calculate the patient's daily energy requirements (kcal/kg/day), priority should be given to enteral nutrition, combined intravenous nutrition or replacement in some cases. Cases such as intolerance or contraindications such as paralytic ileus, intestinal obstruction, vomiting, uncontrolled abdominal pain. Not because of high blood sugar that limits energy supply, blood sugar rise beyond the allowable level should be controlled with insulin until the condition is stable.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
If you have a need for consultation and examination at Vinmec Hospitals under the nationwide health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.