This is an automatically translated article.
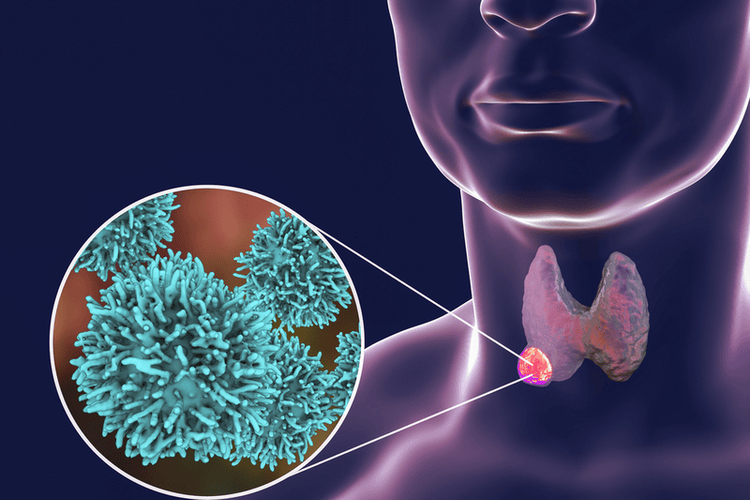
Thyroid hormone has a significant impact on cardiovascular structure and function. Accordingly, cardiovascular complications of hyperthyroidism is also one of the complications on common organ systems in the body when this disease is not detected early and treated properly.
1. Effect of thyroid hormone on cardiovascular hemodynamics
The effects of thyroid hormone on the heart and peripheral blood vessels include a decrease in peripheral resistance and an increase in resting heart rate, thereby increasing left ventricular contractility and afterload. Thyroid hormone reduces resistance in the peripheral arterioles through a direct action on the vessel wall and a decrease in mean arterial pressure. Furthermore, the T3 hormone also increases erythropoietin synthesis, leading to an increase in red blood cell mass. These changes combine to promote an increase in circulating volume in the body, which is between 50% and 300% higher than in the average person. On the other hand, while thyroid hormone in hyperthyroidism is actively working to lower peripheral resistance, which causes mean arterial pressure to decrease, the renin-angiotensin-aldosterone system, which plays a role Important in regulating blood pressure, increasing activity. By increasing salt and water reabsorption, the renin-angiotensin-aldosterone system responds with an increase in blood volume and preload, contributing to an increase in cardiac output.It is the synergy between the function of thyroid hormones and the renin-angiotensin-aldosterone system, resulting in a burden on the cardiovascular system. The myocardium changes in response to increased volume requirements, so in the long run, it will lead to Graves' disease, complications of heart failure. In addition, patients are also at increased risk for cardiovascular complications of hyperthyroidism to varying degrees if the goal of controlling thyroid hormone blood levels is not achieved with hyperthyroidism treatment.
Hormone tuyến giáp ảnh hưởng đến tim mạch gây tăng nhịp tim ở người bệnh
2. Normal cardiovascular response to hyperthyroidism
2.1 Tachycardia Tachycardia with the sinus tachycardia pattern is the most common problem in patients with clinical and subclinical hyperthyroidism. This is the reason why patients go to the doctor because of the feeling of palpitations. Therefore, when 24-hour Holter ECG monitoring shows in young patients a persistently elevated heart rate throughout the day with reduced heart rate variability, the diagnosis of hyperthyroidism should be suspected.
2.2 Volume expansion Volume expansion is a consequence of the effects of thyroid hormone and decreased vascular resistance, tachycardia, and increased myocardial oxygen consumption.
2.3 Reduced exercise capacity Despite the high cardiac output, patients with hyperthyroidism have a markedly reduced endurance during exercise or other demanding activities. This phenomenon is due to increased cardiac activity, which reduces cardiovascular reserve, eventually leading to a decrease in cardiac output during physical exercise. Because the physiological reserve mechanisms of the heart such as increased heart rate, blood volume, and cardiac contractility have been maximally utilized, the capacity to respond to exercise is reduced.

Người bệnh cường giáp bị giảm khả năng gắng sức trong các hoạt động thể lực
3. Cardiovascular complications of hyperthyroidism
3.1 Cardiac Arrhythmia Hyperthyroidism is associated with atrial arrhythmias, dysfunction of the sinus node, and abnormal pulsation. It is the effect of thyroid hormones that increase the activity of arrhythmias, get rid of the inhibition of the sinus node. Patients with untreated hyperthyroidism have a high rate of extrasystoles and are at risk of dangerous arrhythmias and circulatory collapse if not detected and controlled in time.
3.2 Atrial fibrillation Atrial fibrillation is an irregular and often rapid heartbeat. This condition can lead to stroke, which is one of the complications of hyperthyroidism.
Patients at risk of atrial fibrillation due to hyperthyroidism are usually the elderly and those with underlying cardiovascular disease. These subjects often have to be treated with blood thinners to prevent the possibility of blood clots forming in the heart.
3.3 Congestive Heart Failure Congestive heart failure is a condition that can be caused by untreated hyperthyroidism over a long period of time. Because thyroid hormone increases circulating volume, myocardial fibers must increase tone, increase contractility, long-term will lead to heart failure. Congestive heart failure complications of Grave's disease are increased in patients over the age of 60, those with undiagnosed hyperthyroidism, and those with pre-existing cardiovascular disease. Sometimes heart failure can be the first manifestation of hyperthyroidism in elderly patients, while other symptoms of hyperthyroidism are vague.
3.4 Valve Disease The likelihood of valve degeneration is increased and more rapid in patients with basedow disease. Therefore, echocardiography should be indicated periodically in patients with Grave's disease, in order to screen for complications of hyperthyroidism in general or cardiovascular complications of hyperthyroidism in particular, especially in high-risk patients. hearing a murmur in the heart.

Bệnh basedow có thể gây ra biến chứng suy tim sung huyết ở người bệnh
3.5 Hypertension Secondary hypertension is one of the cardiovascular complications of hyperthyroidism. In other words, in patients newly diagnosed with hypertension, especially at a young age, thyroid function testing is necessary. The reason is that sometimes hypertension is the sole symptom of basedow's disease. At the same time, if hypertension is not detected, the long-term coping with increased intra-arterial pressure will lead to Graves disease complicated by heart failure.
3.6 Pulmonary Hypertension The pulmonary artery is a separate blood vessel that carries blood to the heart. While the effects of thyroid hormone increase cardiac output and decrease peripheral resistance, the effects on pulmonary artery pressure are disproportionate, ultimately leading to true pulmonary hypertension.
An increase in pulmonary artery pressure increases the load on the right ventricle, causing the right ventricle to contract with greater force to push blood into the pulmonary vasculature, ultimately leading to increased pulmonary resistance and pulmonary capillary damage . At this time, impaired gas exchange function in the lung parenchyma in patients with concomitant hyperthyroidism should be recognized as a complication of hyperthyroidism.
In summary, hyperthyroidism causes high cardiac output and left ventricular hypertrophy in the early stages, dilation and congestive heart failure in the late stages. This is the mechanism underlying the cardiovascular complications of hyperthyroidism. Accordingly, early treatment and effective control of thyroid hormone are key in preventing the complications of Graves' disease and heart failure.
For detailed advice, please come directly to Vinmec health system or register online HERE.













