This is an automatically translated article.
Myocardial infarction is becoming more and more common as and is one of the leading causes of death for patients. The introduction of early reperfusion methods has reduced the mortality rate from myocardial infarction. However, patients with myocardial infarction may still have adverse events, often arrhythmias, especially ventricular arrhythmias. Let's find out what is arrhythmia in myocardial infarction in the article below.
1. What is arrhythmia in myocardial infarction?
Myocardial infarction is a state of total autonomic dysfunction, which increases the automaticity of the myocardium and conduction system. Along with that, electrolyte disturbances and hypoxemia contribute to the occurrence of arrhythmias in myocardial infarction.
In patients with myocardial infarction, there is an increase in the concentration of catecholamines in the blood, an increase in sympathetic sympathetic activity, etc., which contributes to the development of cardiac arrhythmias.
2. Classification of arrhythmias in myocardial infarction
Cardiac arrhythmias in myocardial infarction can be classified into the following groups:
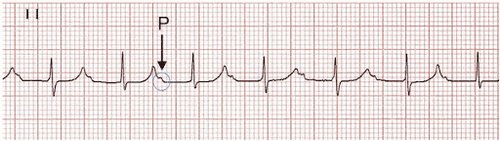
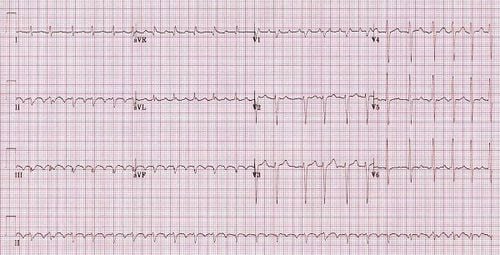
Ventricular tachycardia: Sinus tachycardia, paroxysmal supraventricular tachycardia, atrial flutter, atrial fibrillation. Accelerated coupling tempo. Bradycardia: Includes sinus bradycardia and junctional bradycardia. Atrioventricular block. Block furniture. Ventricular arrhythmias: Ventricular extrasystoles, accelerated ventricular rate, ventricular tachycardia, ventricular fibrillation. Reperfusion arrhythmia. Sinus tachycardia: Associated with increased sympathetic activity, leading to transient increases or decreases in blood pressure. Sinus tachycardia increases myocardial oxygen demand and decreases diastolic time, resulting in decreased circulation and worsening myocardial infarction. Causes of sinus tachycardia such as anxiety, heart failure, pain, hypovolemia, anemia, hypoxemia, pericarditis, pulmonary embolism, etc. Sinus tachycardia needs to be recognized early and appropriate treatment, including analgesia, oxygen supply, diuretics, fluid rehydration, anti-inflammatory, ischemic reduction with beta-blockers, nitroglycerin, ... Atrial ventricular extrasystoles: Usually due to atrial dilation, no specific treatment. Atrial extrasystoles need to be recognized early, through recognition of underlying heart disease, especially heart failure. Paroxysmal supraventricular tachycardia: Occurs about 10% of patients with myocardial infarction. Atrial flutter: Occurs in about 5% of patients with myocardial infarction, usually transient, due to overstimulated atrial sympathetic activity. Atrial fibrillation: accounting for about 10-15% of patients with myocardial infarction, atrial fibrillation is often triggered by heart failure. In the setting of myocardial infarction, pericarditis and conditions that increase left atrial pressure can also lead to atrial fibrillation. Accelerated junctional rhythm: Heart rate about 70-130 beats/min, due to increased automatism of the junctional tissue. Sinus bradycardia: A variable form of cardiac arrhythmia in myocardial infarction. The mechanism is caused by stimulation of afferent vagal receptors in the heart. Atrial - ventricular junction bradycardia: is a protective arrhythmia, the rate is about 35-60 beats/min. First degree atrioventricular block: Found in 15% of patients with myocardial infarction, PR interval >0.2 seconds on electrocardiogram. Second degree atrioventricular block: Mobitz I atrioventricular block occurs in 10% of patients with myocardial infarction. Second-degree atrioventricular block is often associated with QRS stenosis and is most common in inferior myocardial infarction. Mobitz I atrioventricular block does not affect the patient's prognosis and does not require treatment. If heart rate is inadequate, intravenous atropine can be used. Mobitz II atrioventricular block is characterized by wide QRS, associated with anterior myocardial infarction, poor prognosis, often progressing to complete heart block. Therefore, it is necessary to treat Mobitz II AV block immediately with percutaneous pacing or atropin. Third degree atrioventricular block: Or complete heart block, occurs in 5-15% of patients with myocardial infarction. Interior blocks: Conduction of electrical impulses from the bundle of His is transmitted through 3 bundles, the left anterior bundle, the left posterior bundle, and the right bundle. Conduction abnormalities in these bundles are seen in 15% of patients with myocardial infarction. Ventricular extrasystoles: Ventricular extrasystoles are common in patients with myocardial infarction and do not develop into ventricular fibrillation. Accelerated ventricular rate: Found in 20% of patients with myocardial infarction, common in patients with early reperfusion. Characteristic of accelerated autoventricular rhythm on electrocardiogram is wide, regular QRS complex, rate faster than the atrial rate but less than 100 bpm, with atrioventricular dissociation, slow P wave, no conduction, not associated with an enlarged QRS complex. Ventricular tachycardia: Unsustainable ventricular tachycardia: when there are 3 consecutive ventricular tachycardias with a frequency > 100 beats/min and lasts less than 30 seconds. When there are many episodes of unstable ventricular tachycardia, the risk of circulatory collapse is increased. However, unsustainable ventricular tachycardia occurring 48 hours after myocardial infarction in patients with an EF < 40% increases the risk of sudden cardiac death. Therefore, it is necessary to monitor the patient, especially for electrolyte disturbances to promptly handle the situation when the condition is severe. Sustained ventricular tachycardia: : when there are 3 consecutive ventricular tachycardias with a frequency > 100 cycles/min and lasting less than 30 seconds or causing hemodynamic collapse requiring intervention. There is an emergency indication for sustained ventricular tachycardia because it often progresses to ventricular fibrillation and has severe hemodynamic consequences. Ventricular fibrillation: includes early and late ventricular fibrillation. Premature ventricular fibrillation peaks within the first hour after infarction and rapidly declines thereafter. Late ventricular fibrillation occurs 48 hours after infarction and is associated with pump failure and cardiogenic shock. Ventricular tachycardia storm: when there are 3 episodes of ventricular tachycardia, ventricular fibrillation occurs within 24 hours, is a medical emergency, requiring multimodal care. Arrhythmias due to reperfusion: common in patients undergoing percutaneous coronary intervention or thrombolytic therapy and coronary bypass surgery. Arrhythmias due to reperfusion include bradyarrhythmia, accelerated autoventricular rate, ventricular tachycardia, ventricular fibrillation, ...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: www.bvdkquangnam.vn.