This is an automatically translated article.
During the current complicated COVID-19 epidemic, there are many people who are interested in whether the loss of smell is reversible or how to cure the loss of smell after having COVID-19. This article will help you learn about the resilience of loss of smell.
1. Mechanism of loss of smell
The underlying mechanism of odor loss present in COVID-19 continues to be explored as more research is underway. However, several hypotheses and initial observations may explain why loss of smell and taste occurs more frequently in COVID-19 patients even in the absence of other signs of nasal congestion as with SARS. colds and flu.
In a small percentage of people with stuffy and runny nose, physical blockage of the nose with mucus will reduce the odor. However, the majority of COVID-19 patients with loss of smell usually do not have a stuffy or runny nose, so other mechanisms must be involved.
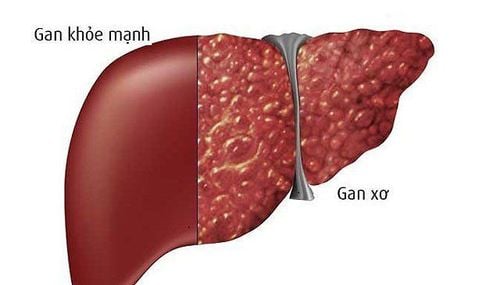
So what can lead to sudden loss of smell during COVID-19? SARS-CoV-2 leads to damage to nerve support cells in the nose that causes loss of smell. There are two types of cells involved, smell receptors and nerve support cells. Early-stage studies also suggest that the virus selectively attacks odor-receptors, which are associated with odor-receptors in the brain, leading to concerns that the virus will follow spread to the brain. However, autopsy showed that SARS-CoV-2 very rarely entered the brain, and the hypothesis that the smell cells were damaged is also uncertain.
When SARS-CoV-2 binds to ACE2/TMPRSS2 on stable cells in the nose, it dies leading to loss of sensory cilia on olfactory receptor neurons. As a result, the odorant will not be able to bind to the cilia of the nerve cells, thereby causing ischemia. All of this can happen very quickly within a day or two.
While this is happening, the stem cells can rapidly regenerate the central cells (usually within 3 to 7 days), allowing the cilia on the olfactory nerve cells to regenerate the odorants again associated with neurons and the sense of smell recovers (in 1 or 2 more days).
A study of 202 COVID-19 patients within 1 month also showed a recovery rate of 49%. But some patients also suffer quite severe damage and there are even cases of prolonged loss of sense of smell, incomplete recovery or a different perception of smell than the one in memory and even a foul, unpleasant odor.
So far, there is no effective treatment for olfactory disorders, but it can be trained, ie, for the patient to practice smelling certain odors so that the nose can relearn the smell.

Rất nhiều người quan tâm đến việc mất khứu giác có hồi phục được không
2. Is the loss of smell reversible?
Loss of smell has become a common symptom in patients with COVID-19. However, that's not the only olfactory dysfunction experienced by people with COVID-19, and even those who have recovered have reported a constant sense of rotting flesh that seems to follow them everywhere. .
Some people even find that normal odors can suddenly turn into rotten, metallic or skunk-like odors. For example, some people wake up every morning to find that the familiar scent of their favorite coffee has been transformed into the stench of garbage or rotting meat.
This syndrome is also known as olfactory / taste disorder (parosmia) – Change in smell perception. A 2021 study found that nearly half of study participants reported having a parosmia condition and 1 confirmed case of COVID-19 restored their sense of smell within about 3 months of recovery. For some people, the condition lasts much longer than that. A young woman recently went viral online about her ongoing experience with parosmia, which began about 10 months ago.
According to medical experts, a disorder of the sense of smell can occur if COVID-19 damages the olfactory receptors in the nose or affects parts of the brain needed for the sense of smell.
3. Why is the loss of smell caused by Covid-19?
According to scientists, Covid-19 has the ability to damage the olfactory system (the connection between the nose and the brain), which perceives odors. The olfactory system can heal on its own, but this process takes time, which can take anywhere from two weeks to two years.
The SARS-CoV-2 virus normally enters cells through the ACE2 receptor (ACE2 gate). The sea urchin protein recognizes the ACE2 receptor, so it attaches quickly and helps the envelope virus to merge into the cell envelope. ACE2 receptors are found in many types of cells in the body, especially those in the respiratory system. This is also the reason why the SARS-CoV-2 virus often enters the body through the respiratory system.
What's interesting is that the olfactory nerve cells located on the inside of the nose have no ACE2 receptors. Therefore, the SARS-CoV-2 virus usually will not be able to attack and infect and damage olfactory cells. However, the olfactory cells will be located between the support cells and these cells have ACE2 receptors. When SARS-CoV-2 enters, these cells will be vulnerable to first attack because they are located in the nose and respiratory tract.
Neural support cells are extremely important in transmitting taste signals to your brain. Damage to these cells makes the olfactory area inactive, not sending nerve signals to the brain, causing loss of smell.
This is good news because nerve support cells can be replaced after your body heals, while damage to nerve cells is often difficult to repair. Therefore, most Covid-19 patients will usually recover their taste for some time after the body is free of Covid-19. About 63% of Covid-19 patients will recover their sense of smell after 5 weeks, and 95% of Covid-19 patients will recover after 6 months. The sooner the Covid-19 respiratory symptoms are treated, the faster the chance of having an odor.

Chữa mất khứu giác bằng cách tập ngửi mùi
4. Cure loss of sense of smell
Treatment of odor loss with drugs Studies on the use of topical corticosteroids in the treatment of acute loss of smell in patients with COVID-19 have not been consistent. Some studies show that the recovery time for the sense of smell is faster, the percentage of patients recovering is higher; however, some other studies did not show a difference compared with the placebo group.
Using topical nasal corticosteroids should only be used to treat loss of smell after 2 weeks for patients with COVID-19 who have a stuffy or runny nose, helping to reduce edema of the nasal mucosa. Aggressive treatment is only instituted when the patient's loss of smell persists for more than 2 weeks.
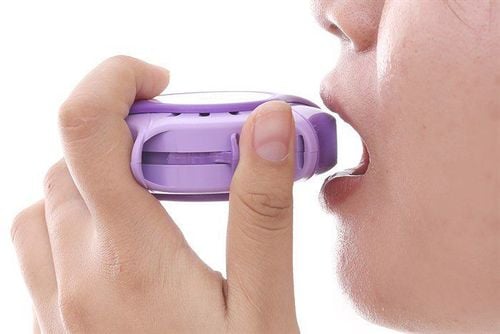
Cure loss of smell by practicing smelling This is a simple olfactory loss treatment, using brain memory in combination with familiar smells to help your body relearn how to smell. Note, the olfactory nerve cells have not been damaged by Covid-19 so we only practice slowly, the smell recovery will be fast.
First, we should learn to smell 4 to 6 smells a day, each time bringing to the nose to smell for 20 to 30 seconds. Then, with your eyes closed, recall the smell that used to be pleasant or unpleasant. Should start with simple, familiar smells, such as perfume, shaving cream, the smell of people around... Then come more specific smells. It is necessary to repeat this exercise several times a day, doing it right at the beginning of the loss of smell will help us recover the smell faster.
This exercise can also be applied and combined with loss of food taste due to Covid-19. We can taste the food and relive it in the past.
Most patients can recover their sense of smell and taste with proper treatment. However, for some people, the sense of smell and taste can be persistent, requiring more specific treatments.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.