This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Venous thrombosis occurs in approximately 20% of pancreatic cancer patients, resulting in significant increases in morbidity, mortality, and healthcare costs. The management of venous thrombosis is particularly challenging in these patients. Adequate selection of the most appropriate anticoagulant for each patient according to current international guidelines is warranted to overcome therapeutic challenges.
1. Rate of venous thrombosis in chemotherapy patients
However, a recent systematic review and meta-analysis of randomized controlled trials with chemotherapy and thromboprophylaxis performed in patients with pancreatic cancer have highlighted that thromboembolic events Venous mass was under-reported in a chemotherapy randomized controlled study. The overall incidence of VTE in chemotherapy studies (n = 13,5694 patients) was 5.9% [95% CI: 3.9-9.0; I2 = 94%] and was significantly lower than the corresponding 16.5% (95% CI: 11.7-23.3; P < 0.001) reported in thromboprophylaxis studies (n = 9.631) patient, I2 = 69%). Importantly, 30 eligible randomized controlled trials (n = 9000 patients) were excluded from this meta-analysis because they did not report venous thromboembolism as an adverse event, which It is quite clear that oncologists lack awareness of the burden of venous thrombosis.
2. Incidence and association with risk factors of venous thrombosis in patients with pancreatic cancer
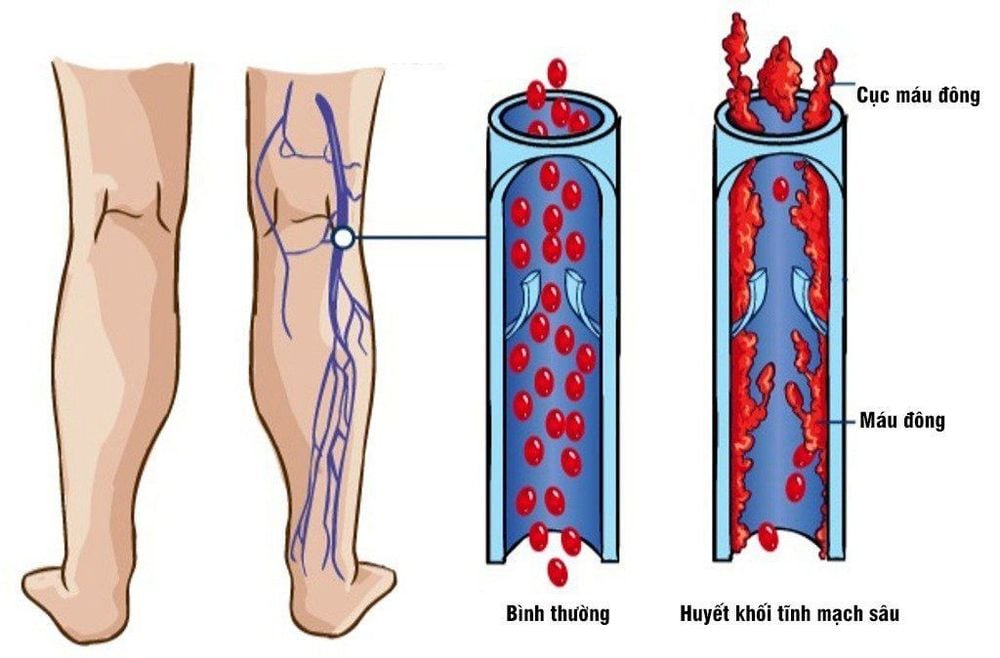
The incidence and risk factors of VTE were recently evaluated in a large prospective multicenter cohort of patients with newly diagnosed pancreatic cancer, providing Modern estimates in real life. In this study, 152 of 731 (20.79%) patients developed a VTE event, with a median time from pancreatic cancer diagnosis to VTE of 4 months. In the competitive risk analysis, the cumulative incidence of VTE was approximately 13% and 20% at 6 months and 1 year, respectively. The most common venous thromboembolic events occurring in patients with pancreatic cancer were deep vein thrombosis (DVT) and pulmonary embolism (PE), but incidental pulmonary embolism and visceral venous thrombosis (PE). VVT) is increasingly being diagnosed, now accounting for about 50% of all reported cases.
3. The relationship between venous thrombosis and mortality
In the BACAP-VVT study, deep vein thrombosis, pulmonary embolism, visceral venous thrombosis, and combined events were observed in 26%, 17%, 30%, and 21% of patients, respectively. Overall, 46% of venous thromboembolism cases were symptomatic and 54% of them were asymptomatic. Initial retrospective studies reported no association between venous thrombosis and survival (OS) in patients with pancreatic cancer. However, all patients included in these studies had metastatic disease with a short lifespan. In contrast, later studies reported that the onset of venous thrombosis was associated with a poorer prognosis. In a retrospective cohort of 227 patients with unresectable pancreatic cancer, venous thrombosis during chemotherapy was associated with a 2.5-fold reduction in progression-free survival (PFS) and 1.6 times the risk of OS disease. Similarly, in a subgroup of 135 pancreatic cancer patients, the onset of venous thrombosis was significantly associated with increased mortality. Importantly, survival was significantly improved in VTE patients treated with anticoagulants compared with those not treated with anticoagulation [hazard coefficient (HR) 0 .30, 95% CI: 0.12-0.74, P = 0.009]. Retrospective studies focusing on randomized venous thrombosis in pancreatic cancer patients also reported an association between visceral venous thrombosis and mortality. Similarly, in a prospective cohort of 731 newly diagnosed pancreatic cancers, patients who developed asymptomatic or symptomatic venous thrombosis during follow-up had significantly shorter PFS (HR) 1.74; 95% CI: 1.19-2.54; P = 0.004) and OS (HR 2.02; 95% CI: 1.57-2.60; P < 0.001) compared with those without venous thrombosis development.
4. Risk factors for venous thromboembolism and risk in patients with pancreatic cancer
Several studies have demonstrated that the most important risk factor for venous thrombosis in patients with pancreatic cancer is the presence of metastatic disease. In a recent retrospective cohort of 165 pancreatic cancer patients, metastatic disease was associated with a 4.8-fold increased risk of venous thrombosis; 41 of 51 patients developed venous thrombosis that had metastasized at diagnosis. Similarly, in the BACAP-venous thrombosis study, metastatic tumors were associated with a 2.5-fold increased risk of venous thromboembolism compared with non-metastatic tumors. Major abdominal surgery is also an important risk factor for venous thrombosis in patients with pancreatic cancer. In an initial observational study of 1915 patients with exocrine pancreatic cancer, 127 of 383 (33.1%) patients requiring pancreatic surgery developed postoperative venous thrombosis. Similarly, 31 of 209 (14.8%) patients requiring pancreatic surgery developed postoperative venous thrombosis in a large retrospective study of 1,115 persons conducted in the East Asian population.

5. Chemotherapy and the risk of venous thrombosis in cancer patients.
However, as recently highlighted by Chiasakul et al., rates of venous thrombosis were not reported in the randomized controlled trial of pancreatic cancer chemotherapy and the respective risk data of these regimens were not reported. Various chemotherapy drugs are still scarce. In recent prospective or retrospective cohorts of pancreatic cancer patients, the incidence of venous thrombosis did not differ between those receiving gemcitabine rapy-based chemotherapy and those receiving FOLFIRINOX.
In the cohort of 273 pancreatic cancer patients included in the Cassini trial, the incidence of venous thrombosis did not differ between patients treated with 5-fluorouracil-based versus gemcitabine-based regimens. . Systematic venous thromboembolism testing is not recommended in daily clinical practice. However, all pancreatic cancer patients must receive oral and written information about the risk factors for venous thrombosis, as well as about the signs and symptoms of venous thrombosis in order to promote promote self-diagnosis and reporting of venous thromboembolic symptoms. Over the past ten years, much effort has been made to develop (data) risk assessment models aimed at selecting cancer patients at highest risk for venous thrombosis, and therefore expected to derive the best benefit from thromboprophylaxis. However, none of these data were designed to specifically assess this risk in patients with pancreatic cancer.
The above information is for reference only, you should consult your doctor before deciding to use any treatment method.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.