This is an automatically translated article.
In autologous stem cell transplantation, the procedure uses the patient's own stem cells for transplantation. After a patient undergoes high-dose chemotherapy, with or without radiation, the stem cells are then returned to the body. This type of transplant is commonly used to treat blood cancers such as Hodgkin's lymphoma, non-Hodgkin's lymphoma, and spinal cord tumors. The following article will provide information about autologous stem cell transplant or bone marrow transplant in the treatment of leukemia.
1. What is Leukemia?
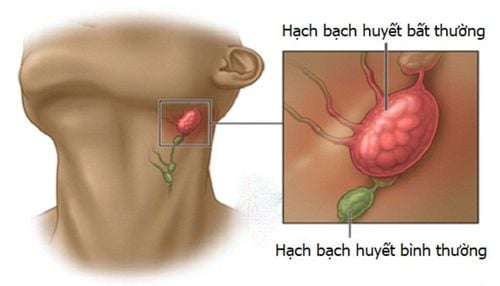
Leukemia is a cancer of the body's blood-forming tissues and it includes the bone marrow and the lymphatic system. This disease has many forms. Some leukemias in children are more common than in adults.
Normally, white blood cells help the body fight infections. However, for people with this condition, the bone marrow makes abnormal white blood cells, which prevents them from working properly.
2. Autologous stem cell transplant, what is a bone marrow transplant?
Bone marrow is the soft, spongy tissue found inside our large bones, like the femur (thigh), hip, and ribs. Bone marrow is made up of cells called hematopoietic stem cells. Hematopoietic cells are given (transplanted) to you during a stem cell transplant. (NOTE: These stem cells are different from the ones used for research - these are embryonic stem cells).
Hematopoietic stem cells are "daughter" cells that become white blood cells, red blood cells or platelets. They may be called hematopoietic stem cells. They grow and are stored in the bone marrow until needed.
Autologous means the transplanted cells come from your own body. Autologous transplantation is also called AUTO transplant or high-dose chemotherapy combined with stem cell infusion.
With the AUTO transplant method, cancer will be treated using the patient's own stem cells. First, stem cells are collected and coagulated. Next, the patient undergoes chemotherapy or sometimes radiation therapy. The previously coagulated stem cells are then thawed and reintroduced into the patient's bloodstream through an intravenous (IV) tube.
After 24 hours the stem cells reach the bone marrow, begin to grow, divide and regenerate healthy blood cells.
Autologous transplants (referred to as “autologous transplants”) are used to treat a number of different cancers, such as leukemia, myeloproliferative syndrome, multiple myeloma, Hodgkin's disease and Hodgkin's disease. , non-Hodgkin lymphoma, testicular cancer, and neuroblastoma, among others.
Some cancers and other diseases prevent the normal development of stem cells. If the stem cells do not develop normally, the blood cells they produce will also be abnormal. So a bone marrow cell transplant will give the body new stem cells. This creates healthy blood cells.
3. How do stem cell transplants work in the treatment of leukemia?
After completing chemotherapy (and radiation if needed), you're ready for your transplant. It does not involve surgery like other types of implants. Instead, your doctor does a stem cell transplant using an intravenous catheter.
Stem cells travel through your bloodstream to reach your bone marrow. There, they make new blood cells to replace the abnormal ones. This process, called incorporation, can take several weeks. You will need to stay in the hospital until your blood cell count returns to a safe level.
Benefits of autologous stem cell transplant? A successful transplant saves many people from getting cancer or delays the progression of cancer.
4. What are the risks associated with autologous stem cell transplantation?
Every step of the stem cell transplant procedure carries risks, including:
Bone pain with growth factor for mobility. Dizziness or tingling in your hands or feet when breathing stops. Side effects of chemotherapy, including pain, fatigue, and nausea. Easy bruising and heavy bleeding. Many people after an autologous stem cell transplant need blood or platelet transfusions. Infections and other diseases until drunkenness occurs. Germs that may not have made you sick before can cause serious complications. Lung problems, including inflammation and pneumonia.
5. Recovery after autologous stem cell transplant?
Until regeneration occurs, your immune system is weak because chemotherapy has destroyed all your blood cells. You face a higher risk of infection, which is why it's important to stay in the hospital for a head start.
When you get home, you may feel tired. Some days, you may feel more like your old self. Other days, you may be too exhausted to get out of bed. It may take several months to fully recover.
You may also face emotional challenges in addition to physical side effects. Unpredictable rebounds can make it difficult to move forward in life. You may worry about whether the transplant will be successful.
In addition, medications that are part of your treatment can affect your appearance and self-image. Talk to your doctor who can help you with additional resources to make this time a little easier.
6. How is autologous stem cell transplant to treat leukemia done?
Stage 1: Collecting patient's stem cells.
During this phase, the patient will be injected with a drug that helps increase the number of stem cells. The treating doctor will collect stem cells through an intravenous tube or catheter placed in a large vein in the chest. The patient is taken in the hospital. Catheters have been used in chemotherapy, other procedures, and blood transfusions.
Time: a few days
Place of action: center or hospital. The patient does not need to stay in the hospital.
Stage 2: Transplant treatment
Once your stem cells have been collected and you know your transplant date, you will go through a process known as preparatory protocol. It is also sometimes referred to as therapeutic or cytotoxic therapy. In this step, doctors use chemotherapy with or without radiation to kill cancer cells.
Time: 5 to 10 days
Place of action: center or hospital. In some transplant centers, patients need to stay in the hospital for treatment, usually about 3 weeks. But for others, patients can come for treatment every day.
Stage 3: Get stem cells back
This stage is also known as stem cell infusion. Technicians retransfuse stem cells into the patient's blood through a grafted catheter.
Time: <30 minutes/transfusion and more than 1 infusion.
Place of implementation: center or hospital.
Stage 4: Recovery
Patient takes antibiotics and some other drugs. If necessary, additional blood will be given. Or will be taken care of by technicians if any side effects occur.
Time: almost 2 weeks. During this time, you will need special protection from infection. Everyone entering the room must wear gloves, a mask and wash their hands with antibacterial soap. Sometimes people entering a room need to cover their clothes with a clean, disposable gown. Fresh fruit, cut plants and flowers are not allowed as they can carry mold and disease-causing bacteria.
Place of implementation: center or hospital. Patient can stay in hospital
7. How to evaluate a successful autologous stem cell transplant
Everyone has different definitions of “successful grafting”. Here are two ways to measure transplant success:
The patient's blood count returns to a safe level. Blood count is the number of red blood cells, white blood cells, and platelets in the blood. A transplant causes a low blood count within 1 to 2 weeks. This increases the risk of:
Infection due to low white blood cell count – white blood cells that fight infection. Bleeding due to low platelet count – platelets help stop bleeding. Fatigue due to low red blood cell count – red blood cells help carry oxygen. The treating doctors will reduce the above risks by transfusion of blood and platelets after transplantation. The patient was also given antibiotics to prevent infection. As the stem cells divide, more blood cells are produced and the blood count improves. That's one way to know if the graft was successful.
Cancer control . Transplant doctors with the main purpose of treating disease. This treatment modality may be appropriate for some cancers such as leukemia and lymphoma. For some patients, remission is the best outcome of treatment. In remission, there will be no signs or symptoms of cancer. After the transplant, the patient needs to see a doctor and do some tests to see if there are still signs of cancer or complications from the transplant.
Vinmec International General Hospital has achieved many achievements in using hematopoietic stem cell transplantation to treat blood and bone marrow cancers. To ensure optimal treatment safety and effectiveness, patients from stem cell transplantation will be transferred to a sterile area for isolation, care and special treatment in an isolation room until their indicators are checked. Post-transplant test returned to normal, then transferred to the normal ward. By this method, many patients with malignant blood diseases have been thoroughly treated at Vinmec.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: oncolink.org, clevelandclinic.org