This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Microscopic colitis is a chronic inflammatory bowel disease, the disease often presents with chronic diarrhea but normal gastrointestinal endoscopy. Therefore, the diagnosis is usually based on histopathology.
1. Classification of microscopic colitis
Microscopic colitis includes two distinct diagnoses, collagenous colitis and lymphocytic colitis. The disease is the name that describes the change in the lining of the colon, but it is not caused by an infection. The disease typically causes chronic, non-bloody diarrhea that affects more women than men.
In some cases, microscopic colitis can be confused with certain diseases such as celiac disease, irritable bowel syndrome, or inflammatory bowel disease.
2. Clinical symptoms
Usually, it is not possible to distinguish between lymphocytic colitis and collagenous colitis. The main symptom is chronic diarrhea (more than 4 weeks), without blood mixed in the stool. The state of watery stools makes the patient feel the need to defecate or have an involuntary bowel movement.
In some severe cases, patients with microscopic colitis may have more than 15 bowel movements per day, but severe dehydration, electrolyte disturbances, and other complications are uncommon. In the advanced stage of the disease, microscopic colitis greatly affects the quality of life of patients. Abdominal pain is also a common symptom of microscopic colitis. Patients often experience discomfort or abdominal pain. However, the differential diagnosis between microscopic colitis and irritable bowel syndrome is difficult.

3. The role of gastroscopy
The definition of microscopic colitis is inflammation of the colon that is diagnosed by histopathology and the patient has a normal colonoscopy. Therefore, total colonoscopy is an important exploratory step in the diagnosis of microscopic colitis. When performing gastroscopy, attention should be paid to detecting colonic mucosal lesions as well as multi-segment biopsies of colon segments. A 2-piece biopsy of each segment of the colon is recommended for a more accurate histopathological diagnosis and biopsies of all segments are more useful than focusing on only one segment. During colonoscopy, the colonoscopy may be normal or near-normal. With the development of endoscopic techniques, mucosal lesions in microscopic colitis have been documented and evaluated as supporting evidence for the diagnosis. A study on patients with collagenous colitis in Japan showed that up to 80% of patients had endoscopic lesions, including: vascular proliferation, unclear mucosal vascular morphology, longitudinal ulcers, Signs of "mucous mucosal inflammation", regional edema, mucosal papules.... In particular, longitudinal streak mucosal lesions have been reported in patients with lansoprazole-associated collagenous colitis. . There have been case reports of collagenous colitis with severe mucosal damage and complications.4. Lymphocytic colitis
Diagnosis of lymphocytic colitis is based on diffuse proliferation of lymphocytes in the epithelial layer (>20 lymphocytes/100 epithelial cells), absence of thickening of the subepithelial collagen band as well as variable change the slot structure.
Lesions of the terminal ileum may be present, characterized by an increased number of lymphocytes on biopsies of the terminal ileum in both patients with lymphocytic and collagenous colitis. In addition, the epithelial layer surface can change the process of proliferation and degeneration, eg appearance of vacuoles, loss of mucin. Compared with normal, there is a diffuse increase in the number of cells in the mucosal stroma. Inflammatory cells appear mainly as lymphocytes, plasma cells but also eosinophils and neutrophils.
5. Histopathological criteria are currently used to diagnose microscopic colitis
In difficult cases, where diagnostic criteria are not met, CD3 staining can be combined to confirm the diagnosis of lymphoid colitis.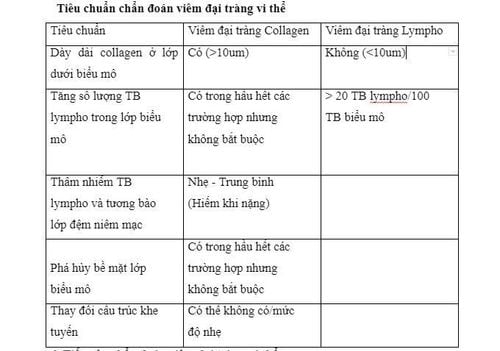
6. Approach to diagnosis of microscopic colitis
The diagnosis of microscopic colitis should be made in all patients with chronic diarrhea. Taking the history will help to differentiate the diagnosis from other diseases in which special attention should be paid to the frequency of defecation and the nature of the stool. Specifically:
Watery stools, a large amount directed to lesions in the small intestine; Moderately loose stools and painful bowel movements are common in cases of lesions in the left colon; Fatty or raw stools suggest malabsorption; Bloody stools suggest inflammatory bowel disease, infectious diseases, or malignancies. The course of symptoms also helps clinicians better orient the cause group. Weight loss may be related to malabsorption, exocrine pancreatic insufficiency, malignancy, or autoimmune disease. Family history of inflammatory bowel disease, Celiac... or systemic symptoms pointing to vasculitis, diabetes mellitus, tuberculosis, lymphoma... should be exploited to make a diagnosis of exclusion. History of drug use, surgery, radiation therapy or dietary factors such as intolerance and allergies should be fully explored.
Microscopic colitis has no typical clinical symptoms but care should be taken to look for symptoms associated with possible autoimmune diseases. The initial steps to help rule out other causes of diarrhea include:
Stool culture for Clostridium difficile, parasites... Complete blood count, electrolytes, protein, blood albumin, erythrocyte sedimentation rate, thyroid function, serological tests to exclude celiac, test for lactose intolerance. Endoscopy and biopsy to confirm the diagnosis of microscopic colitis. In summary, both types of microscopic colitis are characterized by chronic, nonhaemorrhagic diarrhea, watery stools, lymphocyte proliferation, or collagen thickening in the colonic mucosa. The disease is linked to celiac disease, thyroid disease, and diabetes. The primary goals of treatment are to eliminate aggravating factors and control symptoms.
7. Treatment of microscopic colitis
Avoiding risk factors Discuss with the patient the association between smoking, use of certain medications and disease onset and progression.
Using Budesonide is a corticosteroid with local action, the drug is metabolized by the liver, has little systemic effect, so it is very safe. Some other drugs such as: antidiarrheal drugs, probiotics, mesalazine, immunomodulatory drugs.
Have a reasonable diet In nutrition, people with colitis need to avoid eating hot spicy foods, foods that are not hygienic, fast food, foods containing many protective chemicals. management, .... However, many people also wonder about the issue of "can you eat yogurt with colitis or can you drink milk with colitis?". In fact, people with microscopic colitis do not need to avoid eating yogurt, as it provides a good amount of probiotic bacteria, helping the intestines absorb nutrients better.
In summary, microscopic colitis is a chronic inflammatory condition of the colon, the disease often presents with chronic diarrhea but normal gastroscopy. Therefore, the diagnosis is usually based on histopathology.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Lina Vigren, Martin Olesen, et al. An epidemiological study of collagenous colitis in southern Sweden from 2001-2010. World J Gastroenterol. 2012 June 14; 18(22): 2821–2826.
Gianluca Ianiro, Giovanni Cammarota, Luca Valerio, Brigida Eleonora Annicchiarico, Alessandro Milani, Massimo Siciliano and Antonio Gasbarrini. Microscopic colitis . World J Gastroenterol. 2012 November 21; 18(43): 6206-6215.
Jegadeesan. Microscopic colitis. Is it a spectrum of inflammatory bowel disease. World J Gastroenterol. 2013 July 14; 19(26)
Monina F. Pascua, Prashant Kedia, Mark G. Weiner, John Holmes, Jonas Ellenberg, and James D. Lewis, Microscopic colitis and Medication Use .Clin Med Insights Gastroenterol. 2010 May 18; 2010(3): 11–19.
Dao Van Long, Dao Viet Hang. Autoimmune diseases of the gastrointestinal tract. Medical Publishing House Lindstrom C.G. (1976). “Collagenous colitis” with watery diarrhea--a new entity? Pathol Eur, 11(1), 87-89. Read N.W., Krejs G.J., Read M.G. et al. (1980). Chronic diarrhea of unknown origin. Gastroenterology, 78 (2),264-271. Lazenby A. J., Yardley J.H., Giardiello F. M. et al. (1989) Lymphocytic ("microscopic") colitis: a comparative histopathologic study with particular reference to collagenous colitis. Hum Pathol, 20(1) , 18-28. Tong J., Zheng Q., Zheng Q. et al. (2015) Incidence, prevalence, and temporal trends of microscopic colitis: a systematic review and meta-analysis Am J Gastroenterol, 110(2 ),265-276; quiz277. Park Y.S., Baek D.H., Kim W.H. et al. (2011). Clinical Characteristics of Microscopic Colitis in Korea: Prospective Multicenter Study by KASID Gut Liver, 5(2), 181-186.