This is an automatically translated article.
Diabetic foot ulcers are classified as mild, moderate or severe. Gram-positive bacteria, such as Staphylococcus aureus and beta-hemolytic streptococci, are the most common pathogens in previously untreated mild and moderate infections. Severe, chronic, or previously treated infections are often caused by germs. Foot infections are common in diabetics and are at risk for lower limb amputation. Therefore, the use of antibiotics to treat diabetic foot ulcers is of great interest to many people.
1. Diabetic foot ulcers
Foot infections are common in diabetics and are at risk for lower limb amputation. Diabetic foot ulcers are classified as mild, moderate, or severe. Gram-positive bacteria, such as Staphylococcus aureus and beta-hemolytic streptococci, are the most common pathogens in previously untreated mild and moderate infections. Severe, chronic, or previously treated infections are often caused by germs.
The diagnosis of diabetic foot infection is based on clinical signs and symptoms of local inflammation. Infected wounds should be cultured after the wound has been cleaned. Tissue samples obtained by scalpel scraping or bone biopsy are preferred over wound gauze.
Imaging studies are indicated for suspected cases of deep soft tissue pustulosis or osteomyelitis. Optimal management requires aggressive surgery and wound management, effective antibiotic therapy, and correction of metabolic abnormalities (primarily hyperglycemia and arterial insufficiency). No antibiotic treatment is needed for uninfected sores.
In diabetics, any foot infection has the potential to become serious. Diabetic foot infections range in severity from superficial disease to deep bone-related infections. Types of infection include cellulitis, myositis, abscess, necrotizing plantar fasciitis, septic arthritis, tendinitis, and osteomyelitis.
Foot infections are one of the most common and serious complications of diabetes. They are associated with increased frequency and duration of hospitalization as well as the risk of lower limb amputation. Foot ulcers and infections are the leading risk factors for foot amputation. Timely prevention, diagnosis and treatment are necessary to prevent disease, especially amputation.

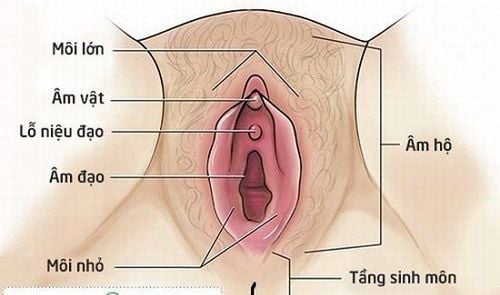
Hình ảnh người bệnh bị loét bàn chân tiểu đường
2. Mechanism of diabetic foot ulcers
Diabetics are particularly susceptible to foot infections due to neuropathy, vascular insufficiency and impaired neutrophil function. Peripheral neuropathy has a central role in the development of foot infections and it occurs in about 30 to 50 percent of patients with diabetes.
Diabetics have reduced or lost sensation for temperature and pain, reducing the perception of trauma such as scratches, blisters or foreign body penetration. Motor neuropathy can lead to foot deformities that contribute to localized pressure from footwear, making the skin more susceptible to ulcers.
Once the skin is damaged (usually on the surface of a plant), the underlying tissues are exposed to invasion by disease-causing organisms. As a result, wound infection may be superficial, but with the delay in treatment and defense mechanisms already impaired by neutrophil dysfunction and vascular failure, it can can spread to subcutaneous tissues and even to deeper structures.
Although most diabetic foot infections begin with an ulcer, focal cellulitis and necrotizing fasciitis can develop without ulceration or trauma.
3. Causes of diabetic foot ulcers
Diabetic foot infections are gram-positive aerobic bacteria, especially Staphylococcus aureus and beta-hemolytic streptococcus (groups A, B, and others).
Infections in patients who have recently been treated with antibiotics or who have deep threatening limb infections or chronic wounds are usually caused by a mixture of Gram-positive aerobic bacteria, gram-negative aerobic organisms (eg, Escherichia coli, Proteus, Klebsiella), and anaerobic organisms (eg, Bacteroides species, Clostridium species, Peptococcus species, and Peptostreptococcus species).
Anaerobic bacteria are often part of mixed infections in patients with foot ischemia or gangrene. Methicillin-resistant S. aureus (MRSA) is a more common pathogen in patients who have been previously hospitalized or who have recently been treated with antibiotics. MRSA infection can also occur in the absence of risk factors because of the increasing prevalence of MRSA infection in the community.
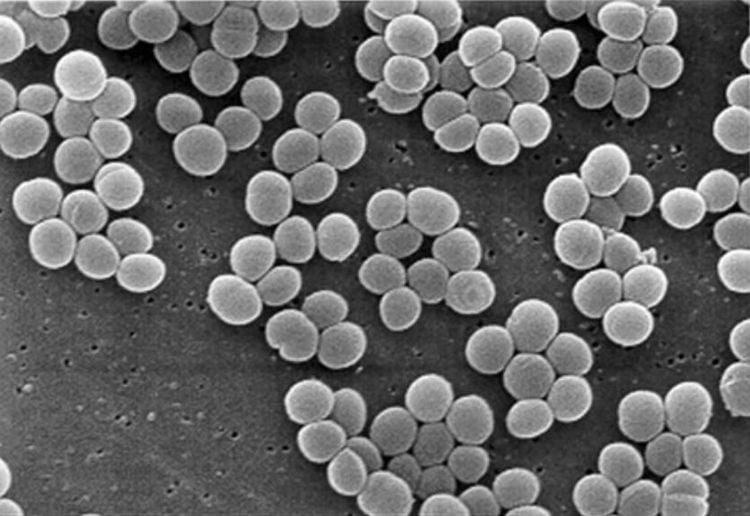
Staphylococcus aureus là một trong các tác nhân gây loét bàn chân tiểu đường
4. Treating Diabetic Foot Ulcers
Effective treatment of diabetic foot infections requires appropriate antibiotic therapy, surgical drainage, excision of dead tissue, appropriate wound care, and correction of metabolic abnormalities.
4.1. Antibiotics for Diabetic Foot Ulcers The choice of antibiotic therapy for diabetic foot infections includes decisions about the choice of empiric antibiotic or the antibiogram, route of administration, and duration of treatment. treatment period.
Initial empiric antibiotic therapy should be based on:
Severity of infection History of recent antibiotic treatment, previous infection with resistant microorganisms. Recent culture results, current Gram-stained detection Patient factors such as drug allergy,... A Gram-stained smear of an appropriate wound specimen can help guide appropriate antibiotic selection. fit. The overall sensitivity of the Gram stain for the identification of organisms growing on culture is 70%. Empiric antibiotic options for diabetic foot infections should always include drugs with activity against S. aureus, including MRSA if needed, and streptococcus.
Patients with mild infections can be treated as outpatients with oral antibiotics including streptococci and staphylococcus aureus. Antibiotic options such as:
Cephalexin, dicloxacillin, amoxicillin-clavulanate, or clindamycin are effective options. If methicillin-resistant S aureus (MRSA) infection is suspected, clindamycin, trimethoprim-sulfamethoxazole, minocycline, or linezolid can be used. If gram-negative and/or anaerobes are suspected, dual therapy with trimethoprim-sulfamethoxazole plus amoxicillin-clavulanate or clindamycin plus a fluoroquinolone such as levofloxacin or moxifloxacin can be used. For moderate to severe infections, patients should be hospitalized for parenteral antibiotic treatment. Empiric options should include streptococci, MRSA, aerobic gram-negative bacilli, and anaerobes. MRSA is killed by vancomycin, linezolid, or daptomycin. Acceptable options for the treatment of gram-negative aerobic organisms and anaerobes include ampicillin-sulbactam, piperacillin-tazobactam, meropenem, or ertapenem.
In addition, ceftriaxone, cefepime, levofloxacin, moxifloxacin, or aztreonam plus metronidazole will be sufficient to kill aerobic and gram-negative bacteria. Tigecycline has been studied, but published experience is limited.
Patients should be re-evaluated 24 to 72 hours after initiating empiric antibiotic therapy to assess response and modify antibiotic regimens if necessary. Several antibiotics have been shown to be effective, but no single regimen has been shown to be superior in the treatment of diabetic foot ulcers.
Antibiotic therapy should not be used for foot ulcers that do not show signs of infection because it does not improve wound healing or prevent infection. Clinical failure of appropriate antibiotic therapy may result from patient non-compliance, antibiotic-resistant bacteria, superinfection, undiagnosed deep abscess or osteomyelitis, or severe tissue ischemia.

Cephalexin là một trong các loại kháng sinh điều trị loét bàn chân tiểu đường
4.2. Duration of antibiotic treatment for diabetic foot ulcers The duration of antibiotic treatment depends on the clinical severity of the ulcer, blood supply to the wound, and response to treatment. Therefore, the duration of treatment should be individualized, depending on the specific patient.
Although there is no clear evidence to inform the optimal duration of antibiotics, the duration of antibiotic therapy is usually indicated as follows:
For patients with mild infections, antibiotic therapy for 5- 5 years. 7 days, combined with wound care, is usually enough to resolve the infection. For patients requiring surgery, intravenous antibiotics should be given for 2-4 weeks after surgery. Then switch from intravenous to oral antibiotics when possible. The duration of antibiotic therapy in osteomyelitis/osteomyelitis depends on the extent of affected tissue remaining after surgery, or if managed nonsurgically. The patient may require amputation of the leg, if all the bones and soft tissues become infected and necrotic. After surgery, the patient needs to use a short course of antibiotic treatment within 2 to 5 days, depending on the clinical condition of the patient.. Where the remaining bone becomes infected after the bone necrosis. destroyed, four to six weeks of antibiotic therapy is appropriate. If necrotic bone remains, several months of antibiotic treatment may be needed to cure the condition. Mild soft tissue infections can be effectively treated with oral antibiotics, including dicloxacillin, cephalexin, and clindamycin. Severe soft tissue infections can be treated initially with intravenous antibiotics with ciprofloxacin plus clindamycin; piperacillin/tazobactam; or imipenem/cilastatin. The risk of infection with methicillin-resistant S. aureus should be considered when choosing a regimen. Antibiotic therapy should last for one to four weeks for soft tissue infections and six to 12 weeks for osteomyelitis and should be followed by culture-guided definitive therapy.
Foot ulcers in diabetics will depend on the patient's condition, and the doctor will recommend conservative and appropriate treatment methods. Therefore, when seeing an injury on the foot, it is necessary to immediately go to a medical facility for examination, advice and appropriate interventions.
To be examined and treated for diabetes, patients can go to Vinmec International General Hospital to be examined by a team of experienced and specialized doctors. The examination will help the doctor accurately classify the type of diabetes, develop a nutritional regimen, monitor and minimize the risks and complications caused by diabetes to ensure the best health for the patient.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: aafp.org, sahealth.sa.gov.au