This is an automatically translated article.
Posted by Specialist Doctor II Pham Thi Khuong - Infectious Doctor - Pediatric Center - Vinmec Times City International Hospital
Anthrax is an acute infectious disease caused by the bacterium Bacillus Anthracis. The disease can be transmitted to humans through contact with sick animals or diseased animal products.
The susceptibility and immunity of anthrax is not clear at present. However, there is some evidence of occult infection in people who are frequently exposed to the causative agent, which can cause a second but very rare disease.
1. Clinical diagnosis of anthrax
Skin anthrax is predominant, accounting for about 95%, respiratory anthrax is less common, accounting for about 5%. Digestive type is rare. Meningococcal manifestations are very rare and are only secondary to septic complications of other forms, so they are not taken seriously.
Clinical symptoms
Anthrax incubation is from a few hours to a few days (3-9 days), but most of it is within 48 hours of exposure.
1.1. Skin anthrax
2020 UpToDate, Inc. and/or its affiliates. All Rights Reserved.

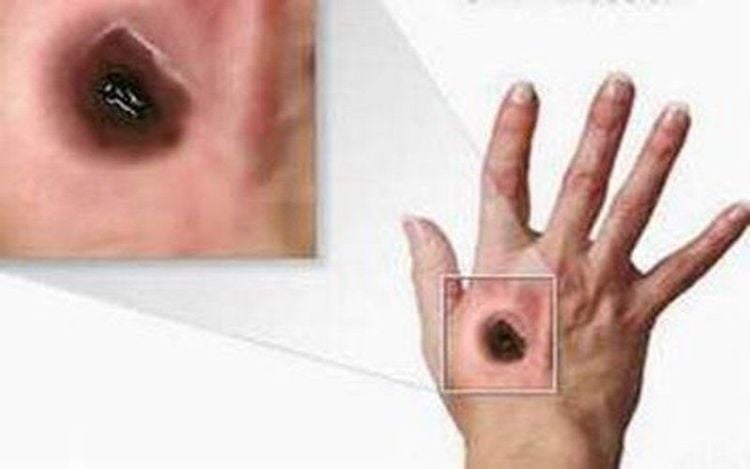
Tổn thương hoại tử với vòng xuất huyết ở bàn tay trái của bệnh nhân bị bệnh than ở da
Reproduced with permission from: Cinquetti G, Banal F, Dupuy A-L, et al. Three related cases of cutaneous anthrax in France. Medicine 2009; 88:371. Copyright © 2009 Lippincott Williams & Wilkins.Hinh1
© 2020 UpToDate, Inc. and/or its affiliates. All Rights Reserved.
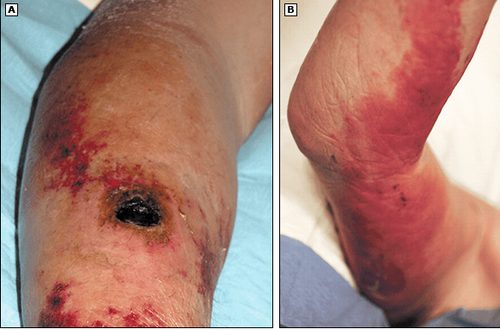
Hình 2: Cutaneous anthrax with lymphangitis
(A) Necrotic wound with associated erythema and edema of the right forearm of a patient with cutaneous anthrax. (B) Lymphangitis with an associated bulla and serous discharge of the medial right arm of the same patient.
Reproduced with permission from: Cinquetti G, Banal F, Dupuy A-L, et al. Three related cases of cutaneous anthrax in France. Medicine 2009; 88:371. Copyright © 2009 Lippincott Williams & Wilkins.
Anthrax is an ulcer, located at the location where pathogens penetrate the skin (usually in open skin: legs, hands, neck, face ...) progressing through stages: macular nodules, nodules, posterior nodules purplish red (blood blisters). The disease causes patients to itch, scratch and burst the blisters, causing widespread death, after 2-4 days forming large ulcers, on the surface covered with a black hard scab. There are many small secondary papules around the ulcer (the "jewel" image). At the ulcer, the patient does not feel pain, even when the needle is inserted. After 3-4 weeks, the ulcer scabs, forming a white scar.
The edema around the ulcer is very strong and widespread. Edema causes compression (edema in the neck and chest causing compression of the trachea...) and signs of "coagulation fibrillation" (Stephanski's sign). Lymph nodes in the area of the ulcer are usually swollen, but painless, and do not turn pus.
Infection syndrome - severe systemic toxicity: Patient has a high fever of 39-400C, chills, fatigue, headache, insomnia... Peripheral blood white blood cells are very high (20,000/mm3).
If left untreated, cutaneous anthrax can be 5-20% fatal. Conversely, if treated, death is rare.
1.2. Respiratory body
Respiratory skin disease has the following symptoms:
Severe infection-toxin syndrome (as if skin). Chest pain, shortness of breath, with pneumonia or bronchial pneumonia, spitting up rust-colored sputum; sometimes pleural effusion or pulmonary edema. Chest X-ray showed enlarged mediastinum due to mediastinal lymphadenitis. Lung parenchyma shows diffuse solidifying infiltrates... Severe: Respiratory failure, cyanosis, shock...
1.3. Digestive body
Digestive anthrax has the following symptoms:
Severe infection-intoxication syndrome. Abdominal pain, vomiting, bloody stools and mucus... Symptoms are similar to those of hemorrhagic necrotizing enterocolitis; sometimes resembles a surgical abdominal emergency (due to mesenteric lymphadenitis...)

Đau bụng là một triệu chứng của bệnh than thể tiêu hóa
2. Definitive diagnosis of anthrax
Based on clinical (mainly skin form), epidemiology, but decisive for diagnosis is specific test including tests: Blood culture for bacteria before antibiotics or reaction test polymerase chain (PCR). Depending on the disease, different specimens will be taken such as:
Pleural fluid, if available for Gram staining, culture and PCR
CSF in patients with meningeal signs, Gram stain, culture and PCR Samples serology in acute and remission for serological testing Pleural and/or bronchial biopsy for testing, if other tests are negative For vesicular lesions, extract vesicular fluid from a vesicle unbroken for Gram staining and culture, or for PCR testing. Gram, and PCR testing In addition, full thickness biopsies of a nodule or vesicle including adjacent skin of all patients must be submitted with 10% formalin for histopathology and histochemistry immunity.
Accordingly, diagnostic tests for patients with suspected gastrointestinal anthrax should be performed as follows:
Ascites fluid for Gram staining, culture and PCR testing Stool or rectal swab for Gram staining, culture and PCR testing Oropharyngeal lesions, if present, for Gram staining, culture, and PCR testing If the patient has surgery, affected tissue can be removed for Gram staining, culture, and PCR testing; Immunohistochemistry can be performed on formalized tissue. Endoscopic staining: (this technique has directional value only). Specimens are blood fluid in anthrax blisters, sputum, urine, feces, vomit, tissue fluid... Gram stain for gram-positive bacteria. Ziehl - Neelson stain to detect spores.
3. Differential diagnosis of anthrax
Skin form of anthrax with plague: Although there are signs of severe infection-infection, swollen lymph nodes, but in plague, lymph nodes are enlarged, painful, purulent and ruptured... Ulcers of anthrax with ulcers in disease Tularemia or staphylococcal ulceration is different from anthrax, Tularemia and staphylococcal ulcer do not have scales, edema is less and only around the ulcer, pain is less... Ulcers of typhus: the same, with black scales , but smaller, no surrounding edema, no secondary blistering, white blood cell usually not increased...
Dựa vào các triệu chứng của bệnh, bác sĩ sẽ chẩn đoán phân biệt bệnh than
4. Anthrax treatment
Anthrax needs to be detected and treated early. Accordingly, it is necessary to isolate the patient in a separate room, the service staff must have gloves and protective boots. Combination therapy with intravenous antibiotics, antitoxins (raxibacumab or anthrax immune globulin), drainage of pleural effusions, supportive care, and adjuvant glucocorticoids is considered in the presence of meningitis.
4.1. Antibiotics
Penicillin G 4,000,000 IU IV every 4-6 hours x 7-10 days or Ciprofloxacin 400mg every 8-12 hours. Tetracycline 0.4 g/time. (or Doxycycline 100 mg) x 4 times/day x 7-10 days.

Thuốc kháng sinh được sử dụng để điều trị bệnh than
4.2. Other alternative antibiotics
Alternative antibiotics such as Amoxicillin, chloramphenicol, or:
Meropenem : In adults: 2 g IV every 8 hours; In children: 120 mg/kg daily in divided doses every 8 hours, not to exceed 2 g per dose. Linezolid: In adults: 600 mg IV every 12 hours; in children <12 years: 30 mg/kg daily in divided doses every 8 hours, not to exceed 600 mg per dose; in children ≥12 years: 30 mg/kg daily in divided doses every 12 hours, not to exceed 600 mg/dose. For respiratory and digestive anthrax, higher doses are required and must be combined with resuscitation. Cardiovascular drugs, water and electrolyte supplements. Besides, do not extract the acne because it is easy to cause bacteremia. If specific Gamma globulin or anti-anthrax serum is available, it may be indicated.
4.3. Hospital discharge criteria
Criteria for patients with anthrax to be discharged from the hospital are as follows:
Clinical recovery: No fever, eating, sleeping, normal activities, normal peripheral blood leukocyte test... For skin type: anthrax has scabbed, healed scars. Two negative bacteriological tests in sputum, stool, and blood, 5 days apart.
5. How to prevent anthrax?
5.1.Common room
The prevention of anthrax needs to ensure the correct animal quarantine regime. Sick animals must not be slaughtered for meat. Animals that die from anthrax must be buried deep, disinfected and disinfected according to regulations...
Workers at slaughterhouses, workshops processing animal products (meat, bones, skin, fur...) It is necessary to strictly comply with the protection regulations, periodically check health, infected skin lesions should be treated well... Disinfection and disinfection of wastes of sick people and animals.

Khám sức khỏe định kỳ sẽ giúp bạn phòng ngừa bệnh than
5.2. Specific disease prevention
Prevention of diseases in humans and high-risk animals with the BioThrax vaccine. Treat exposure with ciprofloxacin (500mg orally twice a day) or doxycycline (100mg twice a day). The duration of post-exposure treatment is more than 6 weeks. Anthrax is a dangerous and rapidly spreading disease. Therefore, the diagnosis, treatment and prevention of the disease should be closely monitored and thoroughly disinfected.
Vinmec International General Hospital is the address for examination, treatment and prevention of diseases. When performing the examination process at Vinmec, customers will be welcomed and used modern facilities and equipment along with perfect medical services under the guidance and advice of experts. Good doctors, well-trained both at home and abroad.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Clinical manifestations and diagnosis of anthrax; Daniel J Sexton, MD This topic last updated: Jan 24, 2019. Tonry JH, Popov SG, Narayanan A, Kashanchi F, Hakami RM, Carpenter C, Bailey C, Chung MC . In vivo murine and in vitro M-like cell models of gastrointestinal anthrax. Microbes Infect. 2013 Jan;15(1):37-44. Epub 2012 Oct 26. Treatment of anthrax; Kenneth H Wilson, MD. This topic last updated: Jan 24, 2019 January 14, 2016,Content source: Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID)