This is an automatically translated article.
Posted by Doctor Ho Thi Xuan Nga - Cardiovascular Center - Vinmec Central Park International General HospitalCoronary artery disease is the most common heart disease encountered in surgical patients. In Western countries, nearly 20% of surgical patients have some degree of coronary artery disease. This rate tends to increase with the worsening of cardiovascular diseases and the aging of the population. In this cohort study, vascular surgery patients occupy a special place. More than 60% of them had signs of coronary artery disease and the postoperative infarction rate was between 4.7 and 8.5%. However, this type has a very high risk of ischemia, accounting for up to 10% of all surgical patients.
1. Coronary artery disease The type, severity, and prevalence of coronary artery disease varies by population. For example, in the case of an abdominal aortic aneurysm, the incidence of clinical angina was 20% in France and 49% in Sweden, and infarction was 16% and 50%, respectively. The incidence of coronary artery disease is zero in Eskimos. In Japan, it is only one-tenth that of Europe and the United States, but the rates of cardiac complications after surgery in these populations do not differ from continent to continent. Response to treatment is also heterogeneous: in North America, for example, black populations respond worse to beta-blockers than white populations.
In general, the relationship between surgical events and postoperative infarction is multifactorial. Many factors are taken into account such as:
Type of population (geography, ethnicity, male or female); Genetic variation in drug response; Importance of sympathetic stimulation and inflammatory syndrome; Associated diseases (diabetes, polyvascular, renal failure); Type of surgery and degree of hemodynamic disturbance; Type of ischemic injury (imbalance between O2 demand and intake or unstable plaque rupture); Quality medical care.

Bệnh lý mạch vành thường nghiêm trọng hơn khi mắc kèm theo một số bệnh lý nền
2. Coronary stenosis 2.1 Pathophysiology of coronary stenosis: Coronary artery stenosis is the result of an atherosclerotic plaque sometimes accompanied by constriction of the heart muscle. Atherosclerosis is a chronic inflammatory response caused by endothelial dysfunction, characterized by excessive levels of C-reactive protein and biochemical stimuli such as LDL (low-weight lipoprotein) cholesterol. in patients who smoke or have diabetes. Endothelial dysfunction is associated with genetic predisposition and stress (hypertension). It leads to the infiltration of low-molecular-weight cholesterol macrophages (foam cells) into vascular smooth muscle cells forming a fibrous cyst that is more or less resistant to rupture on impact, isolating the lesion from blood. These endothelial dysfunction will be accompanied by loss of anticoagulant and vasodilating function, increased activation of local platelet adhesion.
2.2 Stable stenosis and unstable plaque: Coronary artery stenosis is associated with the existence of two types of plaque:
Stable atherosclerotic plaque:
Characterized by a small, lipid-coated central part thick fibromuscular layer, sometimes calcified. It often causes severe (>75 %) stenosis, which is evident on angiography, develops gradually, and restricts blood flow throughout the area, leading to non-Q-infarction with ST-segment elevation.
Responsible for 50-60% of postoperative infarction (highest incidence: after the 3rd postoperative day); Prophylactic treatment: DO2, ↓ MVO2, β-blockers. Unstable atheroma:
Intermittent and irregular growth, consisting of a large central portion of high cholesterol (LDL) fat, in which macrophages and tissue elements mix; This mass is weakly surrounded by a thin layer of fibers (50-65 mcm) showing signs of erosion and scarring. On angiography, this plaque presents with only moderate stenosis (≤50%) and no downstream flow limitation, because it tends to bulge outward and not enter the artery [21]. Its risk depends on its inflammatory activity and its susceptibility to rupture, but not on the degree of narrowing it causes.
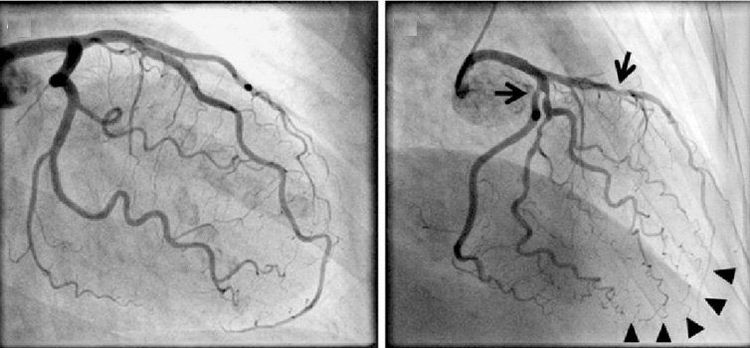
Xơ vữa mạnh vành có thể được phát hiện bằng phương pháp chụp động mạch vành
Less severe stenosis (<60%), no effect on DO2; angina rarely; Insignificant stenosis on angiography, usually negative stress test; Instability, rupture and thrombosis of the artery (ischemia); Leads to infarction with Q waves and ST elevation (STEMI); Responsible for 40-50% of postoperative infarction (<36 hours postoperatively); Prophylactic treatment: antiplatelet drugs, statins. 3. Risk factors for ischemia Degree of flow obstruction in patients with severe, stable stenosis; Unstable degree of an unstable atheroma; The extent and location of the ischemic myocardium; Humoral factors (platelet aggregation, inflammatory syndrome, stress). 4. Myocardial ischemia Ischemia is tissue damage caused by an imbalance between supply (DO2) and demand (VO2) for oxygen, which can be caused by:
Decrease in oxygen supply DO2: spasm blood vessels, narrowing, thromboembolism, hypotension, anemia, hypoxia. An increase in VO2 oxygen demand is associated with: tachycardia, increased wall tension and contractility, tension, pain. Ischemia causes the following events in <5 minutes, in chronological order:
Diastolic dysfunction, Regional hypomotility, Systolic dysfunction, ST changes (ECG), Chest pain (due to adenosine release).
Người bệnh thiếu máu cơ tim có thể xuất hiện các cơn đau ngực
When vascular flow is interrupted > 20 min will cause necrosis (in the absence of accessory circulation). Effects on hemodynamics depend on compromised ventricular mass: 25% cause ventricular failure and > 35% cause cardiogenic shock.
Acute coronary syndromes are defined by the position of the ST segment: elevation (STEMI infarction) or depression (non-STEMI infarction). Infarction is defined by elevation of cardiac enzymes.
Infarction is tissue necrosis occurring 20 minutes after complete coronary occlusion. In the presence of accessory circulation, this period is extended to 4-6 hours. Symptoms are worse if mVO2 is high or systemic blood pressure is low.
Changes in regional hypomobility depend on the thickness of the affected area: 20% cause hypoactivity and ≥ 40% cause immobility. EF is decreased if ≥ 15% of ventricular mass (T) is infarcted. In the acute phase, the area bordering the infarct will increase in size and become reduced or immobile but is able to recover after reperfusion.
There are 2 types of infarction depending on the presence or absence of Q waves on the ECG and on the cause of a stable plaque (DO2/mVO2 imbalance) or an unstable plaque (thrombus).
Clinically in cardiovascular disease: 2/3 of infarctions are due to unstable plaque rupture, (ST elevation > 1 mm, STEMI infarction, presence of Q waves); Postoperatively: 50-60% is due to DO2/mVO2 imbalance (ST depression >1 mm, non-STEMI infarction).
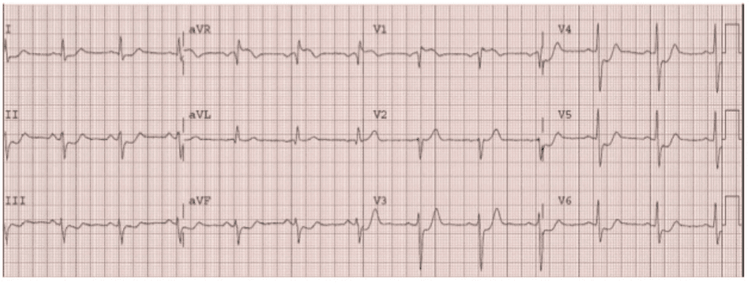
ST chênh lên > 1 mm ở chuyển đạo V1-V3R, V4R
Invite you to see more articles on "Anesthesia resuscitation in ischemic cardiomyopathy and coronary reperfusion" by Doctor Ho Thi Xuan Nga:
Anesthesia resuscitation in ischemic and reperfusion cardiomyopathy Coronary Anesthesia - Part 1 Anesthesia resuscitation in ischemic cardiomyopathy and coronary reperfusion - Part 2 Anesthesia resuscitation in ischemic cardiomyopathy and coronary reperfusion - Part 3
REFERENCES
FLEISHER LA, BECKMAN JA, BROWN KA, et al. ACC/AHA 2007 Guidelines on perioperative cardiovascular evaluation and care for non-cardiac surgery: Executive summary. J Am Coll Cardiol 2007; 50:1707-32 GROSSMAN W, ed. Cardiac catheterization and angiography. 3rd edition. Philadelphia, Lea and Febiger, 1986, 378 KAPLAN Joel.A, Cardiac Anesthesia for cardiac and non-cardiac surgery, 7th edition. Elservier, 2017, 1453-236 KERTAI MD, BOUTIOUKOS M, BOERSMA M, et. Aortic stenosis: An underestimated risk factor for perioperative complications in patients undergoing noncardiac surgery. Am J Med 2004; 116:8-13 KWAK J, ANDRAWES M, GARVIN S, et al. 3D transesophageal echocardiography: a review of recent literature 2007-2009. Curr Opin Anesthesiol 2010; 23:80-8 MILLER FA. Aortic stenosis: Most cases no longer require invasive hemodynamic study. J Am Coll Cardiol 1989; 13:551-8 STS – Society of Thoracic Surgeons National Cardiac Surgery Database, 2005. http://www.sts.org/documents/pdf/STS-ExecutiveSummary.pdf TIMMIS SB, KIRSH MM, MONTGOMERY DG, STARLING MR. Evaluation of left ventricular ejection fraction as a measure of pump performance in patients with chronic mitral regurgitation. Cathet Cardiovasc Intervent 2000; 49:290-7 TORNOS MP, OLONA M, PERMAYER-MIRALDA G, et al. Heart failure after aortic valve replacement for aortic regurgitation: prospective 20-year study. Am Heart J 1998; 136:681-7