This is an automatically translated article.
Articles by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
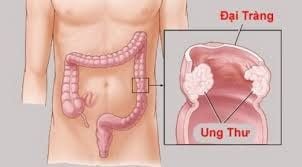
The closer the family relationship between a person and a loved one affected with colorectal cancer, the higher the risk for that person. This is illustrated in analyzes and clinical studies.
1. Family relationship level
The closer the family relationship between a person and a loved one affected with colorectal cancer, the higher the risk for that person. This is illustrated in an analysis of the Nordic Twin Study on Cancer, which found that monozygotic twins of affected twins had a threefold increased risk of colorectal cancer. times that of the general population, while bisexual twins have a 2-fold increased risk.
When evaluating different colorectal cancer family history scenarios, the most common scenario was 1 first-degree relative with colorectal cancer (>90%). Recent evidence suggests that the risk of colorectal cancer in an individual with an affected first-degree relative is independent of the relative's identity. In a large colonoscopy study involving 16 Asia-Pacific regions, colorectal cancer risk (adjusted OR [AOR]] 0.90, 95% CI 0.34–2 .35, P = 0.830), advanced colorectal cancer (AOR 1.07, 95% CI 0.75–1.52, P = 0.714) and colorectal adenomas (AOR 0.96, CI 95 % 0.78–1.19, P = 0.718) in subjects with an affected parent was similar to that of subjects with an affected sibling.
Population-based research in Utah shows that all close relatives of a person with a colorectal cancer index are at increased risk, including first-degree relatives, second-degree relatives, and brothers they first. However, the degree of risk associated with affected second-degree relatives is generally more modest than that observed for first-degree relatives.
In an analysis by Taylor et al., the RR associated with a single second-degree relative (no concurrent first-degree relative) ranged from 1.05 (95% CI 0.99–1.11) to 1.48 (1.11–1.93) with an increasing number of second-degree relatives affected, while RR involves 1 first-degree relative concurrently and at least 1 first-degree relative two ranges from 2.12 (95% CI 1.90–2.35) to 3.37 (95% CI 2.20–4.93).
2. Number of first-degree relatives affected
The literature consistently shows that the higher the number of relatives affected with colorectal cancer, the greater the relative and absolute risk for an individual to develop colorectal cancer. Naber et al.'s cost-effectiveness analysis used a Microscreening Analysis (MISCAN) model to estimate the cost and impact of endoscopic screening strategies with different ages and time periods. each other based on the lifetime colorectal cancer risk estimate input obtained from the studies by Taylor et al. and Fuchs et al.
It is important to note that the study did not take into account the age of affected relatives with colorectal cancer and the high number of first- or first-degree relatives and second-degree relatives (≥2 ) with colorectal cancer or Lynch syndrome-associated cancer should raise suspicion and study for an underlying hereditary colorectal cancer syndrome.
However, the findings suggest that an increasing number of first-degree relatives is associated with an increased lifetime risk of colorectal cancer in all age groups. In the secondary analysis of the PLCO trial by Schoen et al., subjects with 2 first-degree relatives had significantly higher adjusted heart rates for colorectal cancer frequency than those with 1 primary body (2.04; 95% CI 1.44–2.86 vs 1.23; 95% CI 1.07–1.42).

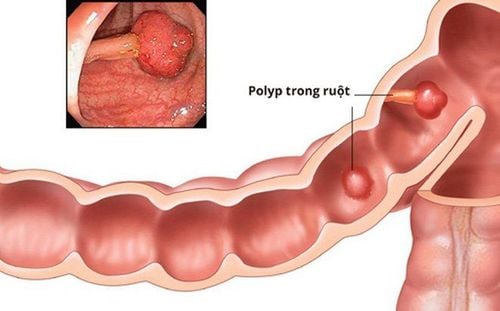
3. Family history of polyps
Many of the limitations observed in familial colorectal cancer risk studies apply to studies evaluating the effect of family history of adenomas. In fact, most studies have evaluated the risk of adenomas in people with a first-degree relative with colorectal cancer, rather than the risk of colorectal cancer in people with a first-degree relative with colorectal cancer. line.
In a prospective study from Hong Kong, Ng et al reported that the prevalence of advanced adenomas was 11.5% among siblings of patients with advanced adenomas, compared with 2, 5% in siblings of those without advanced adenomas (OR 6.05; 95% CI 2.74–13.36). In addition, the prevalence of all colorectal adenomas was significantly higher (39.0% vs 19.0%; OR 3.29; 95% CI 2.16–5.03). A recent study from the same group of investigators found that a family history of undescended adenomas was less associated with advanced adenomas: the prevalence rate of advanced adenomas was 3.9 % of first-degree relatives of individuals with non-growing adenomas, compared with 2.4% of first-degree relatives of individuals with normal colonoscopy (OR 1.67; 95% CI 0.72 -3.91).
A multicenter, multinational prospective study of nearly 12,000 asymptomatic subjects in the Asia-Pacific region found that subjects had at least 1 first-degree relative affected by cancer colorectal cancer is more likely to develop colorectal cancer (AOR range 2.02–7.89), advanced colorectal cancer (AOR range 1.55–2.06), and colorectal adenomas (AOR approximately 2.02–7.89) An AOR of about 1.31–1.92) compared with those with no family history.
Although common adenomas were formerly the main associated colorectal cancer precursor lesions, accumulating evidence suggests that the serrated line is a major contributor to colorectal cancer. Although there are limited data regarding familial risk associated with serrated polyps (other than serrated polyposis syndrome), it is reasonable to include advanced serrated polyps (SSL ≥10 mm, SSL with dysplasia and traditional serrated adenomas) in the broader category of “advanced polyps,” which also includes advanced adenomas, until more data become available.

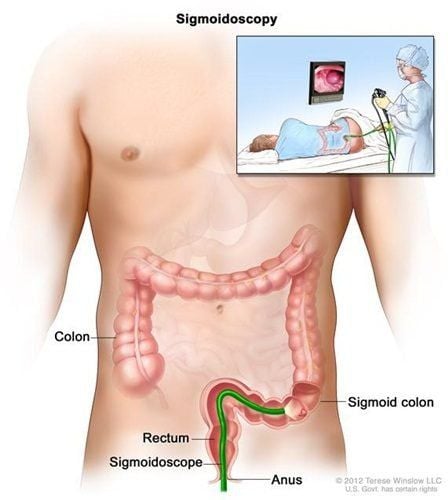
4. Alternatives to colonoscopy in patients with a family history of colorectal cancer
There are no randomized controlled studies comparing the yield and effectiveness of colonoscopy with other colorectal cancer screening modalities specifically for individuals with a family history of cancer colorectal, except for fecal occult blood tests. In a randomized controlled study, investigators randomly selected nearly 1,900 first-degree relatives of colorectal cancer patients for a one-time colonoscopy or three stool occult blood tests. consecutive years. Advanced cancer was detected in 4.2% and 5.6% of first-degree relatives in the fecal occult blood test and colonoscopy, respectively (OR 1.41; 95% CI 0.88–2) ,26) and no colorectal cancer was missed with the fecal occult blood test strategy.
A recent meta-analysis evaluated the performance characteristics of a fecal occult blood test in patients at increased risk of colorectal cancer due to a personal or family history of colorectal cancer. . Subgroup analysis of patients with a family history of colorectal cancer revealed a sensitivity of fecal occult blood test of 86% (95% CI 31%–99%) and specificity of 91% (CI 95). % 89%–93%) for colorectal cancer; for advanced cancer, the sensitivity was 46% (95% CI 37%–56%) and specificity was 93% (95% CI 90%–95%).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Shaukat, Aasma MD et al. ACG Clinical Guidelines: Screening for Colorectal Cancer 2021. American Journal of Gastroenterology: March 2021 - Volume 116 - Issue 3 - pp. 458-479