This is an automatically translated article.
Article written by Doctor Le Van Binh - Intensive care physician - Pediatrics Center - Vinmec Times City International General HospitalAcute respiratory failure is a condition in which the respiratory organs suddenly fail to guarantee the gas exchange function, causing hypoxemia, with or without accompanying hypercapnia (CO2), as demonstrated by the measurement results. Arterial blood gases, with PaO2 < 60 mmHg, PaCO2 > 50 mmHg when breathing with FiO2 = 21%.
1. Causes of acute respiratory failure in children
1.1. Causes of respiratory failure with hypercoaemia
Decreased alveolar ventilation:
Complete airway obstruction: airway foreign body, epiglottitis, laryngitis, laryngeal softening. Increased airway obstruction: HPQ, VTPQ Decreased lung expansion: pulmonary fibrosis, pulmonary edema, interstitial lung disease. Injury to the pleural cavity: Pleural effusion, Pneumothorax. Nerve damage, respiratory muscle damage Increased dead space ventilation:
Increased pulmonary arterial pressure Decreased cardiac output Increased blood CO2 production:
Severe burns Too much sugar
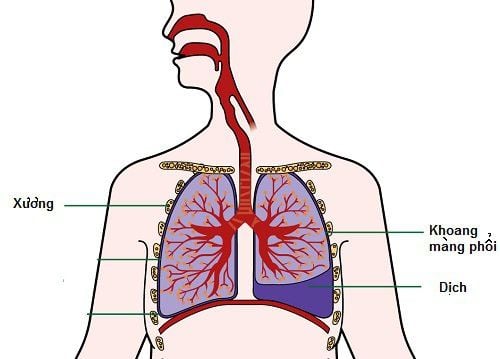
Tràn dịch màng phổi là nguyên nhân gây suy hô hấp có tăng CO2 máu
1.2. Respiratory failure, low blood O2
Intrapulmonary shunt: ARDS, wet pneumonia Change in ventilation-perfusion fraction: meconium aspiration syndrome, cardiogenic pulmonary edema. Intracardiac shunt: right - left shunt Hypoventilation: upper airway obstruction Decreased diffusion: pulmonary fibrosis Decreased venous oxygen pressure: cardiogenic shock
2. Symptoms of acute respiratory failure in children
2.1. Clinical symptoms
Identify the risk of acute respiratory failure
Symptoms of acute respiratory failure are assessed by respiratory rate (sometimes fast, sometimes slow) and breathing effort (evaluate the severity of the disease). Accordingly, respiratory muscle contraction in older children is a sign of severe respiratory failure.
In addition, abnormal breathing sounds are also shown as follows:
Inspiratory stridor: TQ or KQ obstruction. Stridor in both strokes: China obstruction or severe outcome. Expiratory wheezing, prolonged expiration: lower airway obstruction Exhalation groaning: Severe respiratory distress in an infant. Breathing efficiency
Listen to the lungs: Lung silence is a very serious sign. RRPN disproportion suggests cause SHH SpO2 < 92% without oxygen or SpO2 < 95% with oxygen is very severe SHH Consequences of respiratory failure on other organs
Consequences of respiratory failure causing sinus tachycardia, paroxysmal tachycardia, arrhythmia, possibly bradycardia, congestive heart failure. Regarding blood pressure: at first, blood pressure increases to compensate, but if respiratory failure persists or in the end stage, blood pressure decreases. In particular, respiratory failure can cause cardiac arrest due to severe hypoxia or excessive CO2 elevation.
With the condition of the skin, the mucosa lacks O2, making the skin pale due to vasoconstriction, if cyanosis is a late sign, central cyanosis is about to stop breathing. The senses are stimulated, lethargic, comatose, hypotonic. In addition, respiratory failure also affects other organs such as the liver, biliary tract and urinary tract.
2.2. Subclinical symptoms
Arterial blood gas: Helps determine the diagnosis, distinguish the type of respiratory failure, assess the severity, the impact of acute respiratory failure on metabolism, and especially help guide the treatment and management. acute respiratory failure. Arterial blood gas changes in acute respiratory failure: PaO2 < 60 mmHg, SaO2 < 92% and/or, PaCO2 > 50 mmHg, Need to see pH, bicarbonate, residual alkalinity Chest X-ray: indicated for all Patients with respiratory failure to help detect the cause of respiratory failure and distinguish the type of respiratory failure with damage to the lungs, thereby guiding the appropriate treatment. Blood chemistry: Blood chemistry tests often show biochemical disorders, hyperkalemia and hypocalcemia. Blood count: Based on white blood cells, hemoglobin, and platelets. Microbiology: Flu test, nasopharyngeal culture, endotracheal fluid...
3. Treatment of acute respiratory failure in children
3.1 General principles
The general principle of treatment of acute respiratory failure in children is to rapidly normalize O2 and CO2 in the blood, enhancing the effect of the O2 transport system. It also facilitates the repair and healing of lung damage.

Điều trị suy hô hấp cấp ở trẻ cần nhanh chóng bình thường hóa O2 và CO2 trong máu
3.2. Specific treatment
In addition to the general principles of upper respiratory failure, it is necessary to quickly treat and clear the airways with measures: correct posture, aspirate nasopharyngeal fluid,...
Provide oxygen when: The child is pale and/ or SaO2 < 92% and or PaO2 < 60 mmHg of arterial blood gas; Severe thoracic contracture, rapid breathing > 70 breaths/minute.
Oxygen delivery methods:
Normal oxygen delivery method: Nasal oxygen (0.5 - 3 liters / min), Oxygen mask (6 - 8 liters / min), oxygen breathing through a plastic hat (Hood) ( 5 - 8 liters/min) Advanced method of oxygen delivery: If the patient is breathing oxygen normally, but the patient has rapid breathing, severe respiratory muscle contractures, cyanosis, SpO2 decrease < 92% and or PaO2 < 60 mmHg, give oxygen through The mask has a reserve bag of 6 - 10 l/min re-breathing mask (FiO2 60 - 80%), Non-rebreathing mask (FiO2 60 - 100%), Breathe continuous positive nasal pressure (NCPAP). Intubation and mechanical ventilation when failure of O2 through mask or NCPAP / or when the patient is not breathing on their own. Enhance the effect of the O2 transport system
Optimal Hb concentration (> 100g/l): transfusion of red blood cells Ensure cardiac flow: Fluid replacement ensures adequate preload, corrects electrolyte disturbances. Use drugs to increase myocardial contractility, increase blood pressure: Dopamine, Dobutamin, Adrenalin ... Treatment of cardiac arrhythmias (if any) Good oxygen supply in the organization: avoid hypothermia, alkaline blood (when acidosis occurs) Metabolism for sodium bicarbonate according to the formula based on blood gas results: Amount of Sodium Bicarbonate (mEq) = BE x P (kg) x 0.3. Reduce unnecessary oxygen consumption: treat fever, avoid irritation. conditions for the repair and healing of lung damage
Avoid oxygen poisoning: oxygen breathing correctly indicated, method, dose and time of oxygen breathing Adequate nutrition: Should be given by mouth, if not eating placed an hourly nasogastric tube or a basket of gastric drops. Energy needed to increase by 30 - 50% of normal needs due to rapid breathing of children Against superinfection and hospital-acquired infections: Care must be sterile, especially especially when aspirating sputum through endotracheal tract. Reasonable use of antibiotics according to the antibiogram. Specific interventions according to the cause
Remove airway foreign body Aspiration or drainage of fluid/pneumothorax Ensure adequate blood supply. im, blood pressure, reduce pulmonary artery pressure Bronchodilator bronchodilators Respiratory failure can leave dangerous complications, so during the transportation of children, it is necessary to pay attention to opening the airways with a safe position, providing enough oxygen, ensure body temperature and avoid hypoglycemia.
Treatment of respiratory distress syndrome in children is considered a big challenge because this condition requires the baby to be monitored and cared for continuously with appropriate and correct methods. Besides, early hospitalization time is also a decisive factor for success in treatment.
Vinmec International General Hospital is the address for examination, diagnosis and treatment of respiratory failure trusted by many customers. At Vinmec International General Hospital, there is a team of experts, pediatricians, pharmacists and nurses with high qualifications, good expertise, lots of experience, especially dedicated and professional attitude.
Especially with the full support of many modern technical means, Vinmec always ensures to provide the most comprehensive and effective healthcare services.
If you have a need for medical examination by modern and highly effective methods at Vinmec, please register here.
REFERENCES
Guidelines for diagnosis and treatment of some common diseases in children. Ministry of Health - Decision No. 3312/QD-BYT dated 07/08/2015 Advanced Paediatric Life Support: The Practical Approach, Chapter 7 “The structured approach to the seriously ill child”Fifth Edition Australia and New Zealand 2012. , p 207 -218 Texbook of Pediatric Emergency Medecine Update: Acute respiratory distress in children: Emergency evaluation and initial stabilization. This topic last updated: Dec 12, 2016.