This is an automatically translated article.
The article was written by Dr. Hoang Minh Duc - Team Leader of Experimental Production Project, VinmecResearch Institute of Stem Cells and Gene Technology
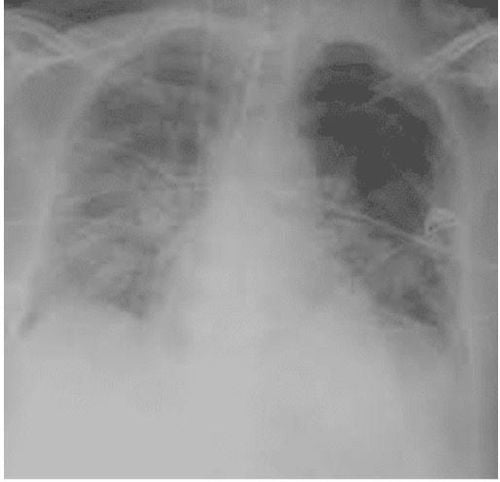
According to Berlin 2012 standards, it is possible to divide ARDS into mild, moderate and severe levels. At the same time, the Conference also made recommendations for treatment corresponding to the severity of the disease, including artificial ventilation strategies, the use of sedatives, muscle relaxants and other supportive treatment measures. .
1. Treatment of acute respiratory distress syndrome caused by COVID-19 virus infection
Non-invasive artificial ventilation is considered indicated for patients with mild ARDS. Pulmonary-protective artificial ventilation remains the primary means of ventilation for degrees of ARDS. This strategy should be combined with low to moderate PEEP in patients with mild ARDS or with moderate to high PEEP in patients with moderate to severe ARDS.
High-frequency artificial ventilation (HFO) and prone position ventilation are indicated for patients with severe ARDS and failure of conventional ventilation. Ventilator muscle relaxants are considered for patients with severe ARDS. Extracorporeal circulatory gas exchange (ECMO) is indicated only in patients with severe ARDS who have failed previous therapies.
2. Stem cell transplant therapy
Stem cells have the ability to replace cells in the body, including lung, blood vessel, and epithelial cells. These undifferentiated cells help the body repair damage, replace damaged cells with new ones, and regulate the immune system, reducing inflammation that has already been initiated.
In several animal models of ARDS and COPD, infusion of human mesenchymal stem cells (TBGTM) derived from bone marrow, adipose tissue, or umbilical cord tissue has reduced disease severity and restored restore lung function.
A report using a 24-h acute lung injury model due to bacterial pneumonia in sheep demonstrated improved oxygenation and decreased extravascular pulmonary fluid in the TBC transplant group compared with the control group without any adverse effects. any side effects.
Moreover, TBGTM-based therapies have demonstrated promising efficacy in the treatment of experimental ARDS through inhibition of alveolar collapse, collagen accumulation, and inhibition of cell death in lung tissue. .
A study also showed that allogeneic stem cell transplantation in 9 patients with ARDS did not have any serious events such as anemia, pneumonia. Recently, Matthay and colleagues conducted a randomized, double-blind, multicenter, randomized trial to evaluate the treatment of allogeneic bone marrow-derived VTE in mechanically ventilated patients with ARDS from the center moderate to heavy.
The results confirmed that stem cell transplantation is safe and due to the low viability of the stem cell products, larger trials are needed to evaluate the treatment efficacy.
A multicenter, double-blind, and placebo-controlled phase II clinical trial (NCT00683722) of CVG transplantation in patients with moderate to severe COPD was conducted between 2008 and 2010 in the United States.
Results showed that during the next 2 years of the trial, no serious adverse events were observed after stem cell transplantation. Another clinical study (NCT01110252) performed in Brazil using autologous bone marrow mononuclear cells (BMMNCs) in COPD patients was performed between 2009 and 2011.

The results of this clinical trial also showed the safety of stem cell therapy as there were no reported side effects associated with stem cell transplantation. Jiaji (2020) published the results of using TMJ to treat 17 patients with ARDS due to H7N9 infection compared with 44 patients as a control group. The results showed that the mortality rate decreased to 17.6% in the stem cell transplant group while the control group was 54.5%.
Among mesenchymal stem cells, umbilical cord-derived mesenchymal stem cells are the most superior. These cells can be isolated from whole sections of the umbilical cord or from individual components of the umbilical cord such as stem cells obtained from arteries and veins, umbilical cord membranes and from WJ mucus masses. .
According to studies comparing the proliferation rate between different mesenchymal cell lines, mesenchymal stem cells from the umbilical cord have a higher proliferative capacity than mesenchymal cells from bone marrow - the cell line is thought to be gold standard for comparison of mesenchymal stem cells or mesenchymal stem cells from adipose tissue or from placental sources.
The average value of the clustering experiment (CFU - colony forming unit) on 1x106 nucleated cells shows that VICELL 1 is capable of generating from 300 to 2000 mesenchymal cell clusters per 1x106 nucleated cells, which is higher. many times mesenchymal cells from bone marrow (range 16-64 clusters per 1x106 nucleated cells).
Some studies on gene intervention techniques show that umbilical cord stem cells still maintain the ability to differentiate after performing gene-altering techniques or after transferring gene fragments into cells by chemical methods. , biological or mechanical. Umbilical cord stem cells carry a gene that activates the production of hepatocyte growth factor (HGF) that can differentiate readily into dopaminergic neurons with the ability to produce dopamine, tyrosine hydroxylase, and several dopamine transporter proteins. These cells were also able to stimulate the self-renewal of nerve cells when transplanted into mice.

Both umbilical cord and bone marrow mesenchymal stem cell lines are also used to evaluate the density of HLA expression on the surface of cells, immune system stimulants and molecules involved. in the process of reducing the immune response.
The results showed that the gene expression of MHCII molecules (including HLA-DMA, -DRA, and –DPB1) in bone marrow mesenchymal stem cells was 16-fold, 36-fold, and 3-fold higher, respectively. times when compared with umbilical cord mesenchymal stem cells. Activation of immune-related genes (including TLR4, TLR3, JAG1, NOTCH2, and NOTCH 1) in bone marrow mesenchymal cells was 4 to 38 times higher when compared with cord stem cells.
These results reinforce the immunostimulatory studies of umbilical cord stem cells and strengthen the database showing that cord umbilical cord stem cells are a mesenchymal stem cell line capable of stimulating the immune system. the lowest immune response of the existing mesenchymal stem cell lines.
The first reason for the immunomodulatory capacity is directly related to the ability to reduce the immune response, even in the case of allografts, due to mesenchymal stem cells in general and umbilical cord stem cells in particular. There are few or no HLA-DRs and MHC-Class I molecules on the cell surface.
Moreover, umbilical cord stem cells do not produce CD80 and CD86 proteins, two proteins that are important in the activation of immune T cells and other T white blood cells.
In the world, FDA has allowed to conduct clinical trials (from phase 1-3) to evaluate the safety and effectiveness of using umbilical cord stem cells in the treatment of clinical diseases. According to clinicaltrial.gov website, umbilical cord stem cell has been used to treat more than 374 diseases ranging from metabolic disorders, immune system disorders to diseases such as Alzheimer's, neurological injuries, diseases. cardiovascular related.
(According to Clinicaltrial.gov statistics, https://clinicaltrials.gov/ ) with more than 115 independent studies worldwide. However, only a handful of these studies have been reported and found to be conclusive.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.