This is an automatically translated article.
Posted by Doctor Le Van Binh Department of Intensive Care - Vinmec Times City International General Hospital
Acute pulmonary edema in children can be caused by many different causes, this is an acute disease, the patient's life can only be saved if the emergency is early and effective.
I. What is acute pulmonary edema?
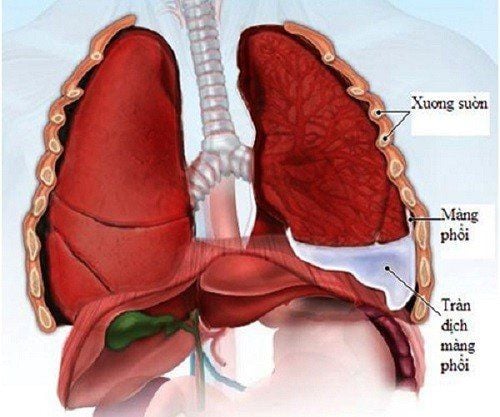
Acute pulmonary edema is a life-threatening medical emergency. Clinical manifestations are left heart failure and respiratory failure. Left ventricular failure causes increased left atrial pressure, increased venous and pulmonary capillary pressure, increased capillary permeability, consequent permeation of fluid into the alveoli, obstructing gas exchange, respiratory failure.
2. Common causes of acute pulmonary edema in children
Some common causes of acute pulmonary edema in children include:
Acute glomerulonephritis High blood pressure Low heart rate: Congenital mitral stenosis Congenital heart with large left - right shunt Overload from perfusion or blood transfusion Acute renal failure or acute exacerbation of chronic kidney failure Myocarditis Hand-foot-and-mouth disease CO poisoning Asphyxiation

Tim bẩm sinh là nguyên nhân gây phù phổi cấp ở trẻ
3. Symptoms of acute pulmonary edema in children
3.1 Conditions suggestive of acute pulmonary edema History: rheumatic heart disease, congenital heart disease, chronic kidney disease History of oligouria, hematuria, and edema suggest acute glomerulonephritis Sudden cardiac failure should suggest inflammation Cardiomyocardial Infusion at a rapid rate suggestive of overload 3.2 Clinical symptoms of acute pulmonary edema Acute pulmonary edema usually appears suddenly and progresses rapidly with the following symptoms:
Cough Shortness of breath, rapid breathing, having to sit breathing Spitting up sputum pink foam Tachycardia Tachycardia Auscultated moist crackles are heard at the bottom of the lungs, typical cases are raised moist rales at the base of the lungs Enlarged liver, distended neck veins High Central venous pressure (CVP) Heart: rhythm gallop or pathological heart sound Severe: palpitations, cyanosis, shock

Trẻ tím tái khi bị phù phổi cấp nặng
4. Differential diagnosis of acute pulmonary edema
Differential diagnosis of acute pulmonary edema with the following pathologies:
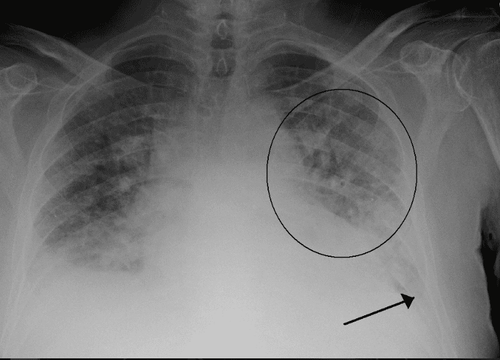
Pneumonia: Fever, cough, dyspnea, crackles, chest X-ray shows pulmonary consolidation. Acute bronchial asthma: History of asthma attack, lungs with rales, chest X-ray shows pulmonary edema. Pulmonary hemorrhage: Bloody sputum, no signs of heart failure, no pulmonary edema on X-ray. Acute respiratory distress syndrome (ARDS): Chest X-ray pulmonary edema, no heart failure, normal CVP.

Chẩn đoán hình ảnh phân biệt phù phổi cấp với các bệnh lý khác
5. How to treat acute pulmonary edema?
5.1 Principles of treatment Reduce cardiac blood volume Respiratory support Drugs that increase myocardial contractility Find and treat the cause 5.2 Specific treatment Stop the infusion if infusion is in progress. Lie on your head 30 degrees. Non-invasive mechanical ventilation (NCPAP): Effective in avoiding end-expiratory alveolar collapse, increasing gas exchange, increasing blood oxygen, reducing intubation rate, and reducing mortality. Increased thoracic pressure reduces blood flow to the heart. Parameters: Starting with a pressure of 4-6 cmH2O and FiO2 of 40-60%, gradually increasing the pressure and FiO2 until there is a response, maximum pressure of 10 cmH2O and FiO2 80%. If NCPAP fails, proceed with intubation to help with balloon ventilation or mechanical ventilation with a PEEP of 6 - 10 cmH2O. If an NCPAP system is not available, the patient can be given 3 to 6 liters of oxygen per minute or oxygen mask with a reserve bag for partial rebreathing. Drugs: Furosemide: Diuretic effect, volume reduction and vasodilation, decreased cardiac blood flow, reduced preload. Doses of 1-2 mg/kg/time IV may be repeated after 2 hours as needed.
Morphin sulfate: Sedative effect, reduce irritability and varicose veins, reduce preload. Contraindicated in patients with hypotension or shock or apnea. Dosage 0.1 - 0.2 mg/kg/time IV. Close respiratory and hemodynamic monitoring (side effects are apnea and shock). Nitroglycerin vasodilator, Isosorbid dinitrate (Risordan): The varicose vein effect reduces preload, in addition, it dilates arterioles and lowers blood pressure. Sublingual tablets act quickly after a few minutes (< 5 minutes). Dose of 0.5 mg/kg/time sublingually repeated every 15-30 minutes as needed.

Điều trị phù phổi cấp bằng thuốc
Inotropic drugs:
In case the patient is not in shock:
Dobutamine: The drug of choice in pulmonary edema. The effect of increasing myocardial contractility and vasodilation reduces preload, the drug does not cause increased heart rate. Initial dose 3 μg/kg/min IV, gradually increasing dose until response, maximum 10 μg/kg/min IV. Digoxin: Indicated in heart failure with tachycardia due to the effect of increasing myocardial contractility and slowing heart rate. Dose for children > 12 months 20 - 40 μg/kg/24 hours IV (1⁄2 doses by slow IV, then 1⁄4 doses at 8 hours and 1⁄4 doses at 16 hours). Phosphodiasterase inhibitor (Milrinon): Indications: Hand, foot and mouth disease with pulmonary edema and high blood pressure. Effects: increase myocardial contractility and peripheral vasodilation to reduce afterload, reduce pulmonary vascular resistance, and reduce preload. Contraindicated in shock. The dose is 0.4 μg/kg/min. In case of shock patient:
Dopamine: Increases myocardial contractility, increases renal perfusion. Start dose 3 μg/kg/min IV and gradually increase dose until response, up to a maximum of 20 μg/kg/min IV.
If you have high blood pressure: Nifedipine (Adalate): 0.2 mg/kg sublingually. Hemodialysis to drain fluid from the body in case of anuria renal failure. Garrot 3 alternating limbs: currently no longer recommended due to: CPAP and the rapid and strong action of diuretics, vasodilators.
Complicated technique, complications of limb lack of perfusion if the technique is not correct.
In acute pulmonary edema due to rapid fluid overload, it usually responds well to fluid arrest, head elevation, NCPAP, ± Dobutamine.
Tiến hành chạy thận nhân tạo rút bớt dịch khi bệnh nhân bị sốc
5.3 Treatment of causes of acute pulmonary edema: Congenital heart failure Rheumatic heart disease Glomerulonephritis 5.4 Follow-up Patients must be closely monitored within the first 24 hours to prevent recurrence of acute pulmonary edema. Monitor: Pulse, blood pressure, respiratory rate, rales, heart rate, SaO2, jugular vein every 5-15 minutes in the first hour. Monitor for three-limb garros if present. Blood gas. See a cardiologist to find and treat the cause. Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in neurological examination and treatment, patients can completely rest in peace. examination and treatment center at the Hospital.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.